Continued from Part 1
Since the two children appear generally intact, you ask your partner to evaluate them more fully while you head for the sedan to find the driver. Anticipating three transports, two stable and one potentially critical, you ask your dispatch to continue the P12, and also to ensure that police are en route (they are).
Arriving at the sedan, you find a middle-aged woman in the driver’s seat, alert. She is pink and warm, perhaps more diaphoretic than you’d expect for the ambient temperature, and does not initially notice as you kneel beside her. A firefighter is holding C-spine immobilization from the back seat.
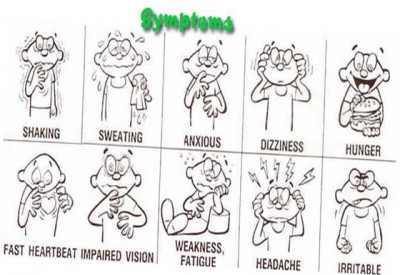
When you greet her and pat her on the shoulder, she gives no response, but with more vigorous stimulation she looks over and acknowledges you distractedly. With multiple attempts and some yelling, you’re able to get answers to a few questions, but she is slow, tangential, and often ignores you outright. She gives her name as Samantha, but cannot or will not provide her last name; she is unable to describe the events that led to the collision; and she gives no medical history or current medications. She does state several times that she’s fine and would like to leave. When asked about her passengers, she mumbles “my kids” and mentions her brother several times. She endorses pain when asked explicitly, but does not specify where. She agrees that she drank “a little” alcohol; when asked about any drug use, she denies it vehemently.
Physically, she appears generally unremarkable. She is breathing somewhat shallowly but effectively, and her radial pulse is around 100 and slightly weak. Her seatbelt is not in place, but it’s unclear whether it was removed at some point. No gross trauma is apparent upon her head, face, or neck, and she does not complain or grimace upon palpation. She is uncooperative with a neurological exam, but demonstrates spontaneous movement of all four extremities. Her pupils are equal and seem appropriately small on this moderately bright day. Chest rise is generally equal and her abdomen is supple; no bruising consistent with seatbelt injury is visible. Her left knee is abraded and somewhat swollen. A sprinkling of dark blotches and streaks are noted on her left ventral arm in the antecubital region. Both frontal airbags are deployed; the windshield is cracked, but lacks a “starred” point of impact; and the plastic dashboard in the driver’s knee area is damaged and cracked. No blood or other damage is visible in the interior compartment. There are no child seats.
Your partner comes over. “The kids seem fine, just upset. One’s complaining of some abdominal pain, but it looks okay. They’re little troopers. Fire says they were wearing regular lap belts with the shoulder strap tucked behind them.”
When you wonder aloud whether there are more patients, he says, “There was nobody else in the car when fire arrived. The truck driver gave a statement to the police about how she was swerving across the road and plowed into him, but then he eloped.” He looks over your shoulder. “Oh, and the P12 is pulling up now.”
What is your treatment plan for these three patients? What are their respective priorities, any points of concern, and how could you shed additional light on their status?
Who will transport which patient, and to which destinations?
What special considerations should be made during documentation?
The conclusion is here




Recent Comments