
So we know now that in any hemorrhagic shock, controlling the bleeding is step one, and restoring the supply of something resembling blood is step two. Should we also consider infusing some other fluids, even those that don’t help carry any oxygen?
Why would we even consider such a thing? It would make sense if “fluid” is what we’re missing, which is the case when shock is caused by something like dehydration. But in hemorrhage, we’re missing blood, not water. Still, there are a few reasons this might be worthwhile. Let’s discuss the “pro” arguments first, then come back around and talk about the “cons.”
The hydraulic argument
Fundamentally, the human vascular system is a hydraulic circuit.
In other words, it’s a giant circle of stretchy elastic tubes, like those long circus balloons. It’s all filled with fluid, which stretches out those tubes and pressurizes the whole system. Then a central pump pushes all the fluid in the system around in an endless loop.
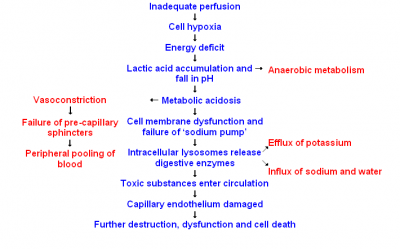
One of the properties of such a system is that, without adequate internal pressure, it won’t work. It’s not that it works badly; it just fails altogether. And although pumping harder and faster can help elevate the pressure a little, and squeezing down on the tubes to make them smaller can help more, in the end if there’s not enough fluid in the system, nothing’s moving anywhere. If the heart isn’t filling with a certain amount of blood during diastole, it won’t push it forward during systole; it can’t pump out what it doesn’t take in.
So maybe there’s a certain logic for maintaining an adequate blood pressure, no matter what sort of fluid we’re actually circulating. Although pressure alone doesn’t carry oxygen, maintaining some pressure is certainly a prerequisite for carrying anything. To put it dryly, although BP isn’t everything, people with no BP are dead.
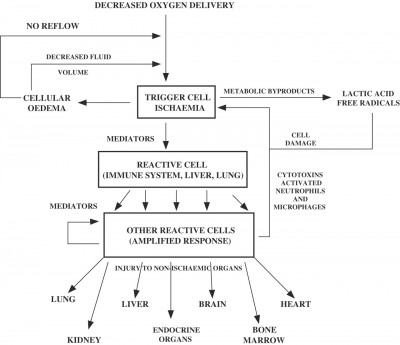
Moreover, some of the pathways in the shock cascade are, perhaps, initiated by low intravascular volume as much as by actual inadequate oxygen delivery. If we can keep the circulating volume pretty decent, maybe we can convince the body that all’s well — no need for a freak-out today.
The extravascular resuscitation argument
Flip back the calendar to the era of the Vietnam War, a landmark time in trauma care. Researchers like Dr. Tom Shires were experimenting on dogs.
They’d do things like drain from them a fixed volume of blood, then clamp off the bleeding and wait for a bit. Then they’d put back every drop of blood they’d removed. Most of the dogs died nonetheless, a phenomenon you and I now understand, since we’re totally experts in the self-sufficiency of the shock process.
But then they’d repeat the experiment. Only this time, rather than just giving the dogs back their blood, they’d also give them some crystalloid fluid. Just water with some stuff like electrolytes in it. This time, more of the dogs survived.
The theory explaining this goes something like so: where is most of the fluid in your body? We know that a high percentage of our bodyweight is water, but does that flow mostly in the blood? Anatomists talk about three different fluid “spaces”: the intravascular space (inside the vessels, where the blood circulates); the intracellular space (the interior of our actual cells); and the interstitial space (the “sea” of fluid permeating the tissue beds but outside the cells, bathing and nourishing them). Fluid moves between these spaces as needed, but at any given time, the majority of your body’s fluid is actually in the interstitial and intracellular (the extravascular) spaces — that is to say, not in the blood at all.
Shock causes increased permeability of the tissues and of the vascular tree, while simultaneously dropping intravascular (hydrostatic) pressure. So when the dogs entered shock, after a short while fluid began to “leak” from the interstitial and intracellular spaces back into the intravascular space. In essence, the dogs’ tissues were returning some of their retained fluid back into the bloodstream — and human tissues do this too. This shift actually increases the vascular volume, which is nice in a sense, and can be seen as a method of compensation: the body is tapping some of its reserve fluid to restore what was lost. However, it does leave the tissues dry. By infusing some saline along with the blood, Shires was helping his test subjects resuscitate both spaces. The intravascular space needed blood, but the extravascular spaces just needed fluid. (Of course, if we replace the blood, eventually the extravascular tissues will be rehydrated and the loaner fluid returned; but if we didn’t provide any extra fluid, that would once again leave the intravascular compartment a little light. Also, some of it — which leaked into neither the intravascular nor extravascular spaces, but the “third space,” areas such as the abdomen where it doesn’t belong — won’t be readily returned at all.)
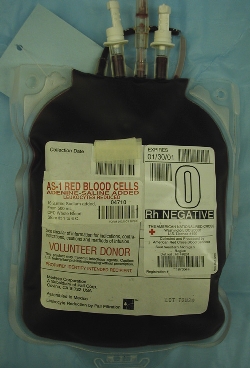
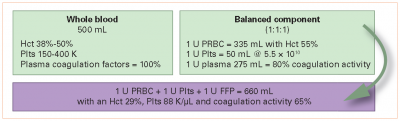
Some combination of these two arguments became the foundation for a decades-long practice whereby hemorrhaging patients are given a certain amount of crystalloid (usually saline, or a modified form of saline like Lactated Ringer’s), often prior or in addition to giving blood products. In many cases this fluid is titrated to maintain a desired blood pressure, and this practice is still widespread today, especially in the prehospital world. In some cases, colloidal fluids (which contain large molecules such as proteins) are also used and have generally similar effects.
Key points:
- Bleeding control and restoring actual oxygen-carrying capacity are the main priorities in hemorrhagic shock, but there may also be value in non-blood fluid resuscitation.
- One argument for this is the maintenance of adequate blood pressure in order for the circulatory system to function.
- Another argument is the replenishment of the fluid lost from extravascular spaces.
Next episode we’ll discuss the dark side of crystalloid resuscitation.
Recent Comments