Continued from Glucometry: Introduction and Glucometry: How to Do it
Implementing glucometry into your overall assessment means understanding three things: when to use it, what the results mean, and when it fails.
Indications
First of all, by and large the only people with derangements of their blood sugar should be diabetics. The rest of us are generally able to maintain euglycemia through our homeostatic mechanisms, except perhaps in critical illness causing organ failure and similar abnormal states. Now, if someone injected you — a non-diabetic — with a syringe of insulin, you’d become terribly hypoglycemic, since it would overwhelm your body’s ability to compensate for the loss of glucose. But nobody’s likely to do that if you’re not a diabetic, unless it’s meant for somebody else and a drug error occurs, or I suppose if they’re trying to assassinate you.
With that said, people walk around who are diabetic and don’t know it. I’ve lost track of the patients I’ve transported who presented with signs suggestive of a diabetic emergency, denied a history of diabetes, and came back with a BGL of 600. Well, my friend, I have some bad news for you. “Everybody is diabetic, even if they’re not” is my attitude. Almost a fifth of older Americans are diagnosed, and the older and sicker they are, the more common it is.
Which brings us back to: who needs a BGL?
The most correct answer is anybody with clinical indications of either hypo- or hyperglycemia. As we saw, diabetes itself is really associated with hyperglycemia, which is why the classic signs of hyperglycemia are usually used to diagnose diabetes: polyuria (excessive urination, as extra glucose is excreted by the kidneys and brings water along with it osmotically), polydipsia (excessive thirst and water consumption, to replace the fluids urinated out), and polyphagia (constant hunger, since despite all the sugar floating around it’s not reaching the cells very easily). If your patient is complaining of those, you might be the first one to discover their condition. The diagnosis doesn’t require elaborate tests and imaging; a fasting glucose over 126 BGL tested on multiple occasions, or just once in combination with clinical symptoms, or a post-prandial (after eating) glucose exceeding 200, is the definition of type II DM. (With that said, I wouldn’t go around diagnosing your patients; that’s not your job, and you’re not quite that good.)
Once the glucose gets higher than the “renal threshold” — usually around 180 in average folks — the body starts to excrete it into the urine. This can actually be detectable by chemical dip-stick, or even by odor and texture at very high levels.
When hyperglycemia becomes severe and prolonged enough, we start to worry about diabetic ketoacidosis. Although burning fat and protein is not necessarily dangerous (some popular diets actually put you into a mild ketogenic state intentionally), extensive accumulation of ketones caused by a total lack of insulin (as in type I diabetics — DKA is rarely seen in type II) creates a metabolic acidosis in the body. This is when the long-term harm of hyperglycemia becomes a short-term hazard. DKA causes altered mental status, usually elevated states of confusion and disorientation, and combative behavior isn’t uncommon. Combined with the acetone odor that sometimes presents on the patient’s breath — which can smell like alcohol — DKA patients can seem suspiciously like drunks, and treating them like drunks is a great way to go down a bad path. (A word of wisdom: not only is everybody diabetic, but drunks are definitely diabetic.) DKA also frequently presents with symptoms of dehydration, due to the osmotic water loss in the urine; nausea and vomiting; and deep, rapid Kussmaul breathing to blow off the acidic CO2.
A few situations can cause short-term hyperglycemia, including stressors of any kind (there’s even “white coat hyperglycemia,” where patients tend to produce elevated sugars at the doctor’s office), but these typically won’t produce anything like the massive levels leading to DKA.
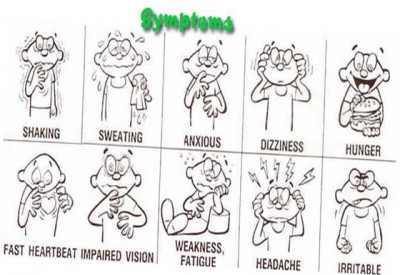
With all of that said, you need to really build up some glucose before hyperglycemia becomes symptomatic, and even more than that before it becomes acutely dangerous and unstable. That’s why as a rule, we’re more concerned with hypoglycemia, usually due to medication administration, physical exertion, or metabolic demand exceeding what was expected. Hypoglycemia again presents as altered mental status, in this case more often an inhibited rather than an elevated state: confusion, lethargy, disorientation, inability to focus or follow commands, weakness, headache, seizures, and eventually coma and death. The fun part is that the impairments can present as focal as well as generalized deficits: unilateral weakness of the limbs or face, speech slurring, poor gait, vision abnormalities, and more. In fact, hypoglycemia is a neurological chameleon, and can look like almost anything; it’s particularly notorious for imitating strokes, and for causing (not imitating) seizures. Interestingly, kids are particularly prone to hypoglycemia due to their gigantic heads, full of glucose-hungry brain.
Despite all this, the primary manifestations of early hypoglycemia are actually not symptoms of hypoglycemia. Rather, they’re caused by catecholamines — by the body releasing stress hormones, primarily epinephrine, in a response to the emergency. (This is not an irrational move: epinephrine helps us release and retain glucose.) As a result, we often seen the same signs we’d expect in anybody with a profound sympathetic stimulus: pale and diaphoretic skin, anxiety and shakiness, tachycardia and hypertension, even dilated pupils. Wise diabetics recognize the early signs of this sympathetic response and drink some Pepsi. As levels keep dropping, these symptoms combine with the neurological effects of glucose starvation to produce a confused, sweaty, increasingly stuporous individual. If left untreated, finally the sugar drops until we’re looking at the picture of impaired and diminished consciousness caused by true hypoglycemia. So just like always, the signs of compensation are our early warning system; once the body decompensates, it’s already late in the game.
To make a long story short, anybody with altered mental status, or any kind of general systemic complaint (weakness, fatigue, anxiety, nausea, etc.) should probably get their glucose tested, whether or not they have a known history of diabetes. This is true even if you suspect another cause, such as stroke. Not only can diabetic emergencies look like anything, they can also be comorbid; it is extremely common for patients to have another problem, yet also to bring a high or low sugar along for the ride, due to the illness throwing a wrench in their normal intrinsic and extrinsic glycemic homeostatic systems.
A number of years ago, there was some limited but compelling research that suggested poorly-controlled blood glucose (meaning not severe derangements but merely small deviations from the ideal range) was associated with increased mortality among an inpatient population with a wide variety of conditions. In other words, if you were hospitalized with something like sepsis, you were more likely to end up dying if your sugar tended to float around 160 instead of 110. As a result, it become trendy to practice extremely tight and aggressive glucose management for virtually everybody; diabetic patients were being tested every few hours and ping-ponged around using medication to keep their numbers textbook-perfect. More recently a number of studies have suggested that this may be less important than was thought, and in fact that excessive paranoia leads to a lot of iatrogenic harm from accidental insulin overdoses. This battle is still being fought in the hospitals, but for our purposes a reasonable take-away would be: when managing acute illness, from sepsis to head injury to cardiac arrest, once everything else is done it’s not a bad idea to check the patient’s sugar.
What’s the Number Mean?
So you’ve taken a blood glucose, either by capillary finger-stick or from a venous sample. Now what?
We mentioned that the “normal” range is something like 70–140. Diabetics seeking to control their condition and not have their toes falling off in a few years usually strive for tighter control of their BGL than is needed for acute care; a sugar of 175 is a little on the high side for a routine check, but a pretty meaningless elevation for our purposes.
All things are also relative, in that a given BGL must be compared to the patient’s baseline to predict its effects. In other words, poorly-controlled diabetics who are routinely sitting at 200 may become symptomatic of hypoglycemia at relatively high levels, whereas very well-controlled diabetics who usually run lower may be able to drop very low indeed without noticing it. However, a few rules-of-thumb are useful:
Non-diabetics usually become noticeably symptomatic below a sugar of, on average, about 53. (Diabetics, particularly those who are usually poorly-controlled, are more variable — their average symptomatic threshold is more like 78.)
After a recent meal, diabetics may demonstrate hyperglycemia to various degrees depending on whether they ate a Cobb salad or an entire chocolate cake. Non-diabetics should not exceed 200 or so. A few people can exhibit hypoglycemia after meals, due to alcohol consumption, “dumping syndrome,” or some other phenomena, but far more often they’ll exhibit similar symptoms without any true hypoglycemia; some people get shaky and sick due to postprandial epinephrine release.
After an unusual period of fasting (“haven’t eaten since yesterday”), non-diabetics should still have a largely unremarkable sugar. For diabetics, it will depend mainly on how much and what type of medication they’re using.
There’s usually a gap of 10–20 mg/dL between hypoglycemia that’s noticeable to the patient (i.e. sympathetic effects) and hypoglycemia that causes cognitive impairment (i.e. neurological changes). This is their safety margin, when they’re taught to eat or drink some fast carbs; if it keeps dropping they may no longer be able to take care of themselves.
But here’s the problem: the sympathetic “warning signs” can be mediated or impaired for various reasons. For one thing, if your body has to flip that switch often, you become numbed to it, and your hypoglycemic thresholds becomes lower and lower. And many patients with various metabolic and endocrine failures simply can’t muster much of a stress response — the same reason why the elderly may not produce tachycardia and other shock signs when they become hypovolemic. Finally, drugs like beta blockers that directly block sympathetic activity can seriously obscure hypoglycemia. Grab your nearest bottle of beta blockers and read the list of adverse effects: one will be hypoglycemic unawareness, a five-dollar term that means beta blockade can make it difficult to know when your sugar drops low.
Another important consideration in evaluating glucose levels is the expected trend. For instance, a BGL of 70 in a diabetic patient might not excite anybody. However, if you’re testing her because her nurse said that she just accidentally received four times her normal insulin dose, then a BGL of 70 should be alarming, because it’s probably going to keep dropping, and she doesn’t have very far to go.
To make a long story short, the clinical effects of both hypo- and hyperglycemia can vary substantially. What to do? It’s simple: assess the patient physically, obtain a history of their oral intake, medications, and metabolic demands (such as exercise), test their sugar if there’s any possibility of glucose derangement, and compare all those data against each other. A low number in the setting of obvious clinical symptoms is bad. A low number in an asymptomatic patient, or a normal number in a patient with highly suggestive signs and symptoms, should force you to bring out your thinking cap and weigh the odds.
What about treatment? Severe hypoglycemia needs ALS or the hospital — they’ll receive IV dextrose. Severe hyperglycemia needs the hospital only, where they’ll receive carefully-dosed insulin; this is generally considered too dangerous to administer in the field (although patients may have their own), so paramedics are reduced to giving fluid boluses, which may help dilute high glucose concentrations (not a very elegant solution) and is probably needed by a patient in DKA anyway, but isn’t really a fix.
What about oral glucose, in the cute little tubes we carry? Typically these are gels containing 15g of glucose, taken orally (either swallowed or held in the mouth — against the cheek or under the tongue — until it’s absorbed). Do they work? Sure. But it’s not much sugar and it’s not very fast. I found one source that suggests 15g of oral glucose should raise the BGL by 50 mg/dL within 15 minutes of administration — but I’ve never found it to be nearly that effective. In my experience, a bump of about 10 mg/dL per tube is about the best you can hope for in the short-term. If you need more than that, go with the medics and the IV syrup.
Testing Errors
When is a tested capillary or venous glucose unreliable? Usually it’s your fault.
Well over 90% of BGLs that test outside the maximum error range (remember, around 15%) are due to user error. Some of the main ones:
- Your meter requires lot coding, and you failed to do so or used strips from the wrong lot.
- You failed to clean the skin before lancing, contaminating the sample (not to mention creating an infection risk), or you had some D50 on your glove and it got mixed in there.
- Rather than gently wicking the sample into the strip, you “smeared” the two together with mechanical pressure, interfering with the expected reaction process.
- You drew blood from an arm with an IV infusion of D50, TPN, or other meds distal to it. Particularly when peripheral perfusion is poor, always try to sample at a different limb from any running drips.
- You tried to reuse a non-reusable strip (gross).
Okay, okay, so nobody’s perfect. Factors that may not be as obvious include:
- Temperature. The test reaction is designed to function within a specific temperature range, which is broad (often around 40–104 degrees) but not limitless, so don’t use them in freezing weather, and try not to leave your equipment ungaraged without climate control when it’s very hot or cold out.
- Altitude. Just in case you’re an Everest expedition doctor.
- Humidity. The strips have trouble when it gets very humid.
- Air. The reagents in the strips will actually degrade if exposed to air for sufficient periods of time, so make sure that you keep them in their tightly-sealed case, and follow their printed expiration dates.
- Time. If you draw whole blood and leave it around (much more likely to happen in the laboratory than in the ambulance), the erythrocytes will metabolize glucose at about 5-7% per hour.
The good news is that in many of these situations, internal error-checking within the glucometer will recognize the problem, and flash an error rather than a reading. Errors messages are usually numbered and can be informative, but each manufacturer uses different codes, so read the manual if you want to know what “ER2” means. (Hint: not enough blood in the sample is by far the most common.) Many of the other problems can be caught if you regularly check the meter using a known-value test solution, which you should be doing anyway according to most drug and safety agreements. (By the way, both the test strips and those vials of solution are usually meant to expire a few months after opening — the printed date is for an unopened bottle — so if they’ve around forever it’s probably time to retire them.)
What about physiological states that can interfere with the reading? We’ve discussed a few, but briefly:
- Hematocrit. Anemia from any cause, including cancer or blood loss, causes falsely high readings. High crit, common in neonates, causes falsely low readings.
- PaO2. Oxygen interferes with the electrochemical redox reaction; thus high concentrations of dissolved oxygen cause falsely low readings, and low PaO2 (i.e. hypoxia) cause falsely high readings, potentially masking a true hypoglycemia.
- pH. Primarily in meters using the glucose oxidase enzyme, alkalosis will cause falsely elevated readings, while acidosis causes falsely low readings. The acidosis of DKA can therefore cause falsely low readings, masking the profound underlying hyperglycemia, so if the clinical picture screams DKA, don’t necessarily let the glucometer tell you different.
- Macronutrients. High levels of circulating proteins or fats can cause falsely low readings due to dilution.
- Hypoperfusion and inadequate circulation. See our previous remarks on this, and remember that venous sources will be more accurate than capillary.
Finally, are there medications that can interfere with glucometer accuracy? There sure are. These in particularly are highly device-dependent, with the glucose oxidase-type meters most often affected. Generally, the effects are not profound, but occasionally they may be clinically relevant.
- Ascorbic acid. Better known as Vitamin C, some people take megadoses of this stuff, thinking it’ll cure their cold or flu. Depending on the meter it can cause falsely high or low readings, usually a minimal change, but at “megadose” levels the effect can be significant.
- Acetaminophen. Also known as Tylenol. The effect is similar to ascorbic acid, but even more modest; it should only be considered in major overdoses, and even then the difference is unlikely to break 35.
- Dopamine. Massive doses, such as might be used for intensive inotropic support, can modestly influence glucose dehydrogenase-based meters.
- Mannitol. High doses can elevated the measured BGL by around 35.
- Icodextrin. This is a dialysate solution used for peritoneal dialysis (not hemodialysis — this is where they pump fluid into the abdomen, let it sit, then drain it out), mainly in patients with diabetes. It metabolizes to maltose, which can cause falsely elevated readings in certain meters. There’s at least one tragic and unfortunate case report of a patient death resulting from massive insulin overdose due to this effect, not noticed until the true BGL was obtained by laboratory analysis. If your patient undergoes peritoneal dialysis, try to find out what dialysate is used, and if that’s not possible, it may be safest to assume their sugar is lower than you’re measuring.
Conclusions
After all this you’re probably thinking glucometry is so convoluted and rife with pitfalls that you’re better off just eyeballing how sweet your patients are. But don’t let me turn you off! This remains one of the best assessment aids we have, because diabetic emergencies remain some of the most common, most treatable, and most easily confused disorders that we encounter. We can’t perform exploratory surgery, and we may never see prehospital CT scans, but this is a diagnostic test that’s so cheap and simple, with such real potential to affect your decisions, that it should be available everywhere. If you maintain your equipment, learn how to do it right, and keep a few basic confounders in mind, it’ll serve you well as one of your most reliable tools.











Recent Comments