To wrap up our story on shock, let’s discuss how to recognize it.
We all have some idea what shock looks like. Like many pathologies, its loudest early markers are actually indirect — we’ll often recognize the body’s reactions to shock rather than the shock itself.
Although there are a few ways to classify the stages of shock, let’s just use three categories here.
Early or Insignificant
Shock that is very early or minimal in effect may have no particular manifestations. One situation where significant or late shock may also be “hidden” is in the elderly patient, or anyone with significant comorbidities; if their body’s ability to mobilize its compensatory mechanisms is poor, then the red flags won’t be as obvious. This doesn’t mean the shock isn’t as bad; in fact, it means that it’s worse, because their body can’t do as much to mitigate it.
The way to recognize shock at this stage is from the history. If we see an obvious bullet hole in the patient’s chest, and three liters of blood pooling on the ground beside him, then it doesn’t matter how the patient presents otherwise; we’re going to assume that shock is a concern. Blood volume is proportional to bodyweight, but for a typical adult, a fair rule of thumb is to assume about 5-7 liters of total volume. (Not sure what a liter looks like? The bags of saline the medics usually carry are a liter; so are those Nalgene water bottles many people drink from. “Party size” soda bottles are two liters.) Losing more than a liter or two rapidly is difficult to compensate for.
Remember, of course, that blood can also be lost internally, and aside from the occasional pelvic fracture or hemothorax, the best environment for this is the abdomen. Always examine and palpate the abdomen of the trauma patient, looking for rigidity, tenderness, or distention. Remember also that the GI tract is a great place to lose blood; be sure to ask your medical patients about blood or “coffee grounds” (old blood) in the vomit or stool.
Fluid enters and leaves the body continuously, and any disruption in this should be recognized. If a patient complains “I haven’t been able to eat or drink anything in two days,” they’re telling you that they haven’t taken in any fluid for 48 hours. If they tell you they’ve been vomiting or experiencing profuse diarrhea, that’s fluid leaving their body in significant volumes. What about the man who just ran a marathon and sweated out a gallon? Did he drink a gallon to replace it?
Compensated Shock
Significant shock will result in the body attempting to compensate for the low blood volume. Much of this work is done by the sympathetic system, and there are two primary effects: vasoconstriction and cardiac stimulation.
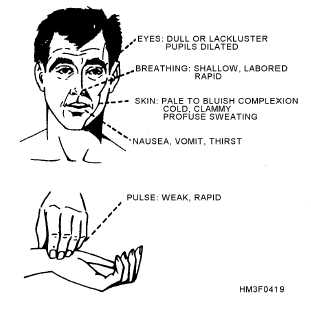
By constricting the blood vessels, we can maintain a reasonable blood pressure and adequate flow even with a smaller circulating volume. We normally vasoconstrict in the periphery — particularly the outer extremities and skin — “stealing” blood from those less-important tissues and retaining it in the vital core. This causes pallor (paleness) and coolness of the external skin. The sympathetic stimulation may also cause diaphoresis (sweating), which is not compensatory, but simply a side effect of the adrenergic release.
The heart also kicks into overdrive, trying to keep the remaining volume moving faster to make up for the loss. It beats faster (chronotropy) and harder (inotropy), resulting in tachycardia. Note that patients who use beta blockers (such as metoprolol) may not be able to muster much, if any, compensatory tachycardia.
A narrowing pulse pressure (the difference between the systolic and diastolic numbers) may be noted; since the diastolic reflects baseline pressure and the systolic reflects the added pressure created by the pumping of the heart, a narrow pulse pressure suggests that cardiac output is diminishing (due to loss of preload), and that more and more of the pressure we’re seeing is simply produced by shrinking the vasculature.
Tachypnea (rapid respirations) are also typically seen. In some cases, this may be due to emotional excitement, and there is also a longstanding belief that it reflects the body’s attempts to “blow off” carbon dioxide and reduce the acidosis created by anaerobic metabolism. (Interestingly, lactate — a byproduct of anaerobic metabolism — can be measured by lab tests, and is also a sign of shock, particularly useful in sepsis.) Additionally, it ensures that all remaining blood has the greatest possible oxygenation. However, it is also plausible that this tachypnea serves to assist the circulatory system: by creating negative pressure in the thorax (the “suction” you make in your chest whenever you inhale) and positive pressure in the abdomen (due to the diaphragm dropping down), you “milk” the vena cava upward during inspiration, improving venous return to the heart and allowing greater cardiac output. This “bellows” effect helps the heart fill more and expel more with each beat.
The more functional the patient’s body is — such as the young, strong, healthy victim — the more effective these compensatory systems will be. Hence the old truism that pediatric patients “fall off a cliff” — they may look great even up through quite profound levels of shock, due to their excellent ability to compensate, then when they finally run out of room they’re already so far in the hole that they become rapidly unhinged. It’s great that these people can compensate well, but it does mean we need to have a high index of suspicion, looking closely for signs of compensation (such as tachycardia) rather than outright signs of shock — because by the time the latter appears, it may be very late indeed.
Patients in compensated shock may become orthostatic; their bodies are capable of perfusing well in more horizontal postures, but when gravity pulls their remaining blood away from the core, this added challenge makes the hypovolemia noticeable. Less acute shock due to causes like dehydration may result in dry skin (particularly the mucus membranes; try examining the inside of the lower eyelid) with poor turgor (pinch a “tent” out of their skin and release it; does it snap back quickly or sluggishly?), and potentially with complaints of thirst. Urine output will usually be minimal. Generally, the more gradually the hypovolemia sets in, the more gradually it can be safely corrected; it’s the sudden, acute losses from causes like bleeding that we’re most worried about.
Decompensated Shock
As shock continues, compensatory systems will struggle harder and harder to maintain perfusion and pressure. Eventually they will fail; further vasoconstriction will reduce rather than improve organ perfusion, beating the heart faster will expel less rather than more blood, and the blood pressure will start to drop.
The hallmark of this stage of shock is the normal functioning of the body beginning to fail. The measured blood pressure will decrease and eventually become unobtainable. Pulses will weaken until they cannot be palpated. As perfusion to the brain decreases, the patient’s mental status will deteriorate. Heart rate and respirations, previously rapid, will begin to slow as the body loses the ability to drive them; like a government office that can’t pay its workers, the regulatory systems that should be fighting the problem begin to shutter their own operations. As the heart continues to “brady down,” eventually it may lose coherence (ventricular fibrillation), or keep stoically trying to contract until the last, but lose all effective output due to the lack of available blood (PEA). Cardiac arrest ensues, with dismal chances for resuscitation.
Alternative Forms of Shock
Although we have focused so far on hypovolemic shock, particularly of traumatic etiology, there are other possibilities. A wide range of shock types exist, but speaking broadly, there are only two other categories important to us: distributive, and cardiogenic/obstructive.
Distributive shocks include anaphylactic, septic, and neurogenic. The essential difference here is that rather than any loss of fluid, the vasculature has simply expanded. Rather than squeezing down on the blood volume to maintain an appropriate pressure, the veins and arteries have gone “slack,” and control of the circulating volume has been lost; it’s simply puddled, like standing water in a sewer pipe. (Depending on the type of shock there may also be some true fluid losses due to edema and third-spacing.) Imagine tying your shoes: in order to stay securely on your feet, the laces need to be pulled snugly (not too tight, not too loose). If the knot comes undone and the laces lose their tension, the shoe will likely slip right off. Your foot hasn’t gotten smaller, but the shoe needs to be hugging it properly to stay in place, and it’s no longer doing its job.
The hallmark of distributive shock is hyperemic (flush or highly perfused) rather than constricted peripheral circulation. The visible skin is warm (or hot) and pink (or red), and the patient may be profoundly orthostatic. Septic shock is associated with infection; anaphylactic with an allergic trigger; and neurogenic with an injury to the spinal cord.
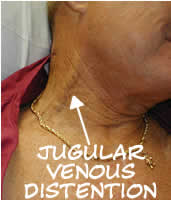
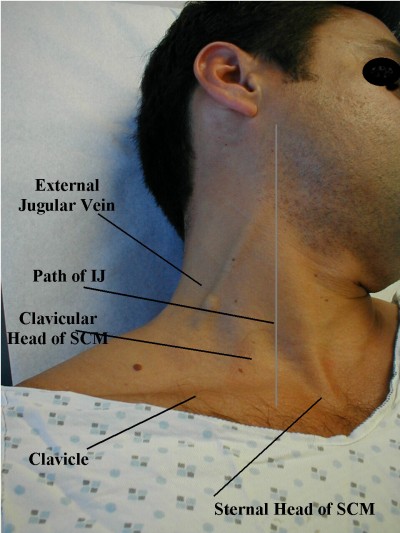
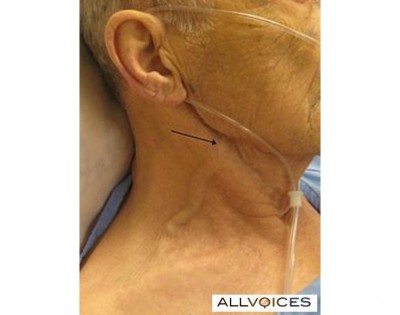
Cardiogenic and obstructive shocks are a different story. In this case, there’s nothing wrong with the circulating volume, or with the vasculature it flows within; instead, there’s a problem with the pump. Cardiogenic shock typically refers to situations like a post-MI heart that’s no longer pumping effectively. Obstructive shock refers to the special cases of pericardial tamponade, massive pulmonary embolism, or tension pneumothorax: physical forces are preventing the heart from expanding or blood from entering it, and hence (despite an otherwise functional myocardium) it’s unable to pump anything out. In either case, we can expect a clinical picture generally similar to hypovolemic shock, but likely with cardiac irregularities — such as ischemic changes or loss of QRS amplitude on the ECG, irregularity or slowing of the pulse, or changes in heart tone (such as muffling) upon auscultation. Pulsus paradoxus (a drop in blood pressure — usually detected by the strength of the palpable pulses — during the inspiratory phase of breathing), electrical alternans (alternating QRS amplitudes on the ECG), and jugular vein distention also may be present in the case of tamponade or severe tension pneumothorax.
In sum, remember these general points:
- The history and clinical context should be enough to make you suspect shock even without other signs or symptoms.
- The faster the onset, the more urgent the situation; acute shock needs acute care.
- Look both for signs of compensation (such as tachycardia) and for signs of decompensation (such as falling blood pressure). However, remember that due to confounding factors (such as particularly effective or ineffective compensatory ability, or pharmacological beta blockade), any or all of these may be absent.
- Distributive shocks are mainly characterized by well-perfused peripheral skin; cardiogenic/obstructive shocks are characterized by cardiac irregularities.
Interested parties can stay tuned for a brief appendix discussing fluid choices for resuscitation — otherwise, this journey through shock is finally finished!
Go to Part X (appendix) or back to Part VIII


Recent Comments