The first, the last, and always the most important answer to the shock progression is to fix the underlying cause.
To illustrate the principles, let’s focus for the moment on traumatic shock caused by hemorrhage — you were injured, began to bleed, and now you’ve got less intravascular blood. What should we do about that? Stop the bleeding? Give you more blood?
If you’re caught in a sudden rainstorm, should your first reaction be toweling yourself off, or getting under shelter?
Both will be needed, but one will be futile without the other.
Shock caused by bleeding is cured by stopping the bleeding. The body will try to do this on its own, but definitively, in significant trauma, this is almost always accomplished through surgery. Trauma is a surgical disease; its medicine is an operating room, sutures, and cautery.
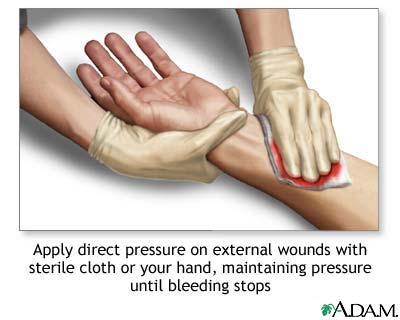
Prior to that, just about anything we can do to stop or slow the bleeding is worth doing. Direct pressure on an injury is often very effective. Pressure slows the flow of blood and promotes the clotting process (by creating stasis and degranulating platelets). It most often fails when it can’t be properly applied — such as when the bleeding is internal, as with a lacerated abdominal organ.
Tourniquets for extremity injuries are perhaps the most definitive pre-surgical intervention of all, and despite years of demonization they have been shown to be generally effective in most cases, with relatively minor risks. More discussion of tourniquets will come another day.
To contrast, consider the counter-example of septic shock. The initial insult there is an infection. How do we treat infection? Antibiotics. Early antibiotic therapy is so important for the sepsis patient that the time from hospital arrival to administration of antibiotics is recorded, and measured in minutes.
The takeaway:
- The prime directive in correcting shock is reversing the original cause; this takes precedence over any other treatment.
- In trauma, this means stopping the bleeding; that usually means surgery, and before that, direct pressure or tourniquets.
- Achieving this control is absolutely essential and absolutely time-critical.
Thanks for this extensive review, I’m enjoying it.
It’s not the focus of your post, but the image at the top spurred to share one note about direct pressure that wasn’t emphasized in any of my EMS classes.You may have picked it up somewhere along the way, but the key to holding pressure is ensuring that the direct pressure applied is truly “direct.”
Obviously some wounds may be large enough to warrant coverage by an entire hand, or more, but in many cases the source of ongoing bleeding can be localized to one or two culprit vessels, e.g. an arterial or venous “bleeder.” If you use two fingers and a single 4×4 to apply pressure directly to a troublesome vessel or small wound, you’re going to get far better hemostasis than if you use your entire hand with a pile of gauze on it.
It’s simply physics. Pressure = Force/Area. Apply the same force over a smaller area, and the pressure will increase.
This is why I’m so glad that when I was taught it, we weren’t told simply to apply “direct pressure.” Instead, it was described to us as “well-aimed direct pressure.”