Location: St. Vincent’s ED
Time: 14:32 Tuesday
Conditions: Light fog
Equipment: fully stocked except 1 child BP cuff (broken) and 1 short splint
Dispatch
You brought a patient into St. V’s half an hour ago, and after handing them off and banging out your report, you’re sitting in their tiny EMS room, jawing away with Steve and the crew of the A13. They just told you about the psych patient they brought in, and you’re firing back with the story of the call you ran last night — a little old lady who managed to keep locking herself behind different doors while everybody ran in circles.
“So then we get into the bathroom, but when we look up, she’s halfway out the –”
The radio on your shoulder crackles, and although it’s turned almost all the way down, you hear:
“Ambulance 61 on the air?”
You stop and look around, grimacing. “Tell them no,” Steve grumps.
Sighing, you click on. “61, go ahead.”
“Are you available?”
“61… sure, show us available from St. V’s.”
After a pause, they crackle back at you (click for audio):
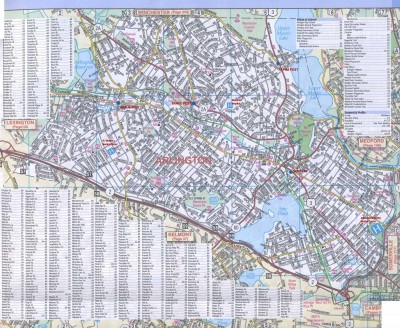
[Ambulance 61, respond priority 1 to 101 Coolidge Rd. 1-0-1 Coolidge Rd, between Gray St and Hawthorne Ave. Paramedic 16 requesting assistance with a chest pain. 61?]
Response
Making your good-byes, you pile out and hop into your truck. “Who’s on the 16?” you ask as Steve pulls into the road.
“Uh… Joe and Jinny? No, she’s on maternity still. Must be Joe and that new guy.”
“They can’t handle a chest pain? What are they doing, massaging his feet?”
“Maybe it’s not Joe… he never calls for BLS. Unless they’re about to code or something.”
By the time you’ve worked it out, you’re on Coolidge Rd. Immediately, you notice the flashing lights of the P16, pulled up to the curb in front of a three-story home. Steve parks a short way behind and calls you on scene over the radio.
Scene
Hopping out, you trot over to their truck and pop open the rear doors. The stretcher is there, but nobody is inside.
“Must be up there,” Steve notes.
“Thank you, Lieutenant Obvious.”
You click onto the radio. “P16, A61?”
After a moment, they come back through heavy static. “16.”
“We’re outside now; do you need anything?”
“Negative, just stand by, we’re coming down now.”
“Copy.”
Steve pulls out their stretcher. “Medics stairchairing? What world is this?”
Together, you roll over to the base of the stairs, drop the stretcher and set it up. A few seconds later, two figures appear at the front door, carrying a middle-aged woman in a stairchair. When they reach the bottom, you wave cheerfully.
It’s not Joe, but the new kid that he’s been working with, plus somebody you don’t know well — a recent hire with experience in an outside system. “Hi guys.”
“Hey.”
You smile at the patient. “Hey there. I’m Sam, this is Steve; we’re the pros from Dover.”
The new guy grunts. “Let’s get her over.”
She’s pretty big — perhaps 250lb — so you wait to see how they want to handle it. They answer your question by holding out a hand and assisting her to stand and pivot to the stretcher. You get her settled then roll her over to their truck. In a few moments, she’s secured inside, and you all pile in.
“Whaddya need?” you ask.
New guy is sitting on the bench, rubbing his palms on his pants and looking a little nervous. His partner has parked his butt on the tech seat and doesn’t look too interested. The patient is a little pale, moist, and appears short of breath, but she offers you a game smile.
“Can you throw her on the monitor?” new guy asks.
“Sure,” says Steve, who’s at the patient’s right side. It’s a BLS-permitted skill when assisting medics in your state. He pulls out the wires and start sticking on electrodes. New guy starts playing with IVs, and his partner is peering at pill bottles to compile a med list.
You actually don’t approve of this sort of thing — medics waiting until they reach their “office” to start their workup — chest pain patients should have their first 12-lead at the bedside — but nobody asked you. You slip on some gloves and shut the rear doors behind you.
“Want a bag?” you ask.
“Yeah, thanks.”
You grab a liter bag of saline and a macro dripset, spike one into the other, and flush the air from the line. Then you hang the bag from a hook overhead and dangle the tubing somewhere clean. New guy is still poking at veins, so you grab a 10ml saline flush and screw it into a lock; you flush that too and leave it in the package nearby.
Steve has the electrodes attached. “Print one?” he asks.
“Yes please. Then the 12-lead if you could.”
He prints a few seconds of a rhythm strip, then halts it, plugs in the 12-lead extension, and begins sticking on yet more electrodes. She’s still wearing her blouse, so he uses fourth-dimensional magic to snake around armholes and neckholes.
You’ve got little to do, so you clip on the pulse ox probe — 90%. “You guys want some oxygen?”
New guy looks up. “Uh, sure.”
You find a nasal cannula, gently secure it to the patient, and start running it at 4 liters. After a minute, the monitor bumps up to 96% saturation.
He’s finally managed to stick a vein, so you hand him the lock to screw into the hub, then a Tegaderm dressing. He hands you back the used catheter; “Grab a sugar off that?”
You pull out the glucometer and milk a drop of blood onto the test strip. “143.”
Steve has everything hooked up, and prints off a 12-lead. Looking across the truck, you can see gross ST elevation in the anterior leads. Not that anybody asked you.
“Okay guys, let’s get going,” new guy announces. “If you could just drive for us please. St. V’s.”
Steve hops out the side door and you step out the back. Pausing at the threshold, you ask, “St. V’s?”
“Yep.”
Well, all right. You slide into the driver’s seat and buckle up. Behind you, Steve is doing the same in the 61. You zero the odometer and stick your head into the compartment: “You guys all set?”
“Yeah, go ahead.”
You pop the truck into gear and start rolling that way, leaving the lights on. Steve follows with the flow of traffic and no blinkeys or wailies. Keying the company radio, you hail, “Operations, P16.”
“Operations.”
“16’s transporting one patient to St. V’s, with the 61.”
“Copy, one to St. Vincent’s, both units.”
You tool along at a quick but reasonable pace. Since you started working with Steve, you rarely drive anymore, so you’re a little rusty, but you can still dodge a pothole with the best of them. From the back, you hear the transplanted medic calling in a notification: “St. V’s, Scenarioville P16, we’re en route with a 67-year-old female, A&Ox4, complaining of 10/10 chest pain, radiating to the left jaw, onset over the past hour, cool and diaphoretic, vomited once. History of CAD with one stent placed. BP 134/88. She’s on oxygen at 4 liters, aspirin’s given, we’re administering nitro now… normal sinus on the monitor, there’s elevation in V2, V3, V4, V5 on the monitor, depression in leads II, III, aVF. Allergic to penicillin, coming in hot. Questions or orders?”
You can’t hear the reply. A few minutes later, you’re pulling into the bay. “Operations, P16.”
“Go for Operations.”
“On arrival at St. V’s.”
“Copy, you’re arriving. 15:01.”
You walk around to the rear doors and pull them open. Inside, the medics are arranging tubes and wires, trying to find a place for everything on the stretcher. You twiddle your thumbs until they finally give you a thumbs up; you draw the stretcher out slowly to ensure nothing snags, and then head inside.
“Room 3,” somebody calls as you show up near the nurse’s station. You back into the room, match up the beds, and start plucking electrodes off the patient’s chest. Once she’s free, you slide her across on the sheet. While you’re getting her situated, the medic gives a report outside. You bid goodbye and get the stretcher out of the way.
In the hall, you start cleaning off the gear, putting it back together and remaking the stretcher. Steve shows up a few minutes later to give you a hand. Once it’s all set, you pop it back into the P16. The older medic is inside, and has things nearly tidied up.
“Thanks,” he grunts. You give him a nod and escape to your own truck.
As Steve pulls out, you ask the obvious. “What on earth did they need us for?”
“New guy nerves,” he mutters. “Partner who doesn’t care.”
“They didn’t even call a STEMI alert on the radio, they just kinda hinted at it. Not that Vincent’s would’ve activated anyway, probably. She’s just going to sit in there until the doc wraps his head around everything and calls the team.”
He shrugs. “That’s what happens when you have an ALS truck without local ALS experience. They should go back to promoting medics from the ranks only.”
You rub your temples and sigh. “Yeah, maybe.”
Discussion
Diagnosis: ST elevation myocardial infaction — 95% LAD occlusion
A typical call intercepting with an ALS unit to assist and drive. Specific ALS skills an EMT-B is permitted to assist with vary by region and service (and depending on the specific providers, the line may be fudged); in this case, Scenarioville BLS can set up IV dripsets and flushes, attach and record ECGs, and several other skills at the direction of a medic. Beyond that, they’re generally there to drive (so that both medics can remain in back, for labor-intensive patients or those who may become so) and function as overall helpers.
Speak Your Mind