There are many, many, many, many, many, many drugs.
And I think it’s noble and wise for a sharp EMT-B to learn as much as he can about as many of them as he can. General mechanism, typical routes, notable adverse effects and contraindications. The most common meds are encountered so frequently that you can’t help but become familiar with them.
But what about all the rest? (You remember those — many, many, many, etc.) Memorize them all? Maybe, but that’s a task on par with memorizing the map of London. I’ll freely admit that my own mental encyclopedia of pharmacology is weaker than it should be.
Use a reference? These are certainly handy; printed quick-books are available, as are digital versions you can access with a smartphone (Epocrates and Medscape are a couple good ones — see the Droid Medic for guidance). But we really ought to have at least a surface recognition of most drugs we come across, without having to consult an Ouija board.
Fortunately, 80-90% of the drugs you’ll encounter can be broadly categorized into a few major types. If you understand these types, and their basic physiological behavior, you’ll understand most of what’s relevant to your care; and it’s easy business to memorize which type a drug belongs to. So let’s go over some of these categories.
Some of these groups seem to fall naturally into matched opposites. So today, let’s discuss…
Stimulants and Depressants
Basically, it’s all about speeding up, or slowing down.
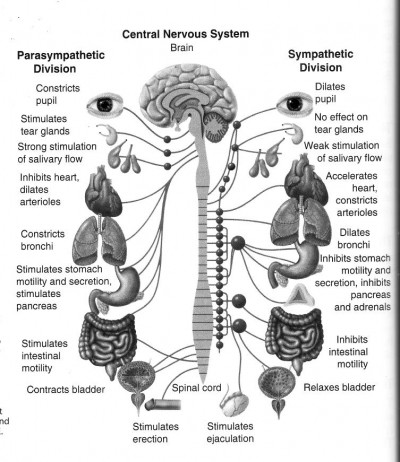
Most of us have heard of the “fight or flight” response, our body’s instinctive ability to step on the gas in times of need — an acute stress response that lets us climb trees, hunt mammoths, and escape from tigers. It’s the get-up-and-go state, and its physiological trigger is known to laymen as adrenaline. This is partly correct; in actuality, your body creates this high-output condition through a variety of hormonal mediators (including adrenaline, more commonly known in the US as epinephrine, but also dopamine and norepinephrine). Overall, this functionality of your autonomic nervous system is known as the sympathetic system.
Some of us have also heard of the reverse state of fight-or-flight, often called “rest and digest” (or sometimes “breed and feed”). This is the slow down, recover, repair, rebuild, and relax state; this is the brake to the sympathetic’s gas. Although slowing down is the last thing you want when escaping from sabre-toothed tigers, it’s just the ticket when you’re enjoying supper or having a snooze. This side of things is known as the parasympathetic system.
(How to keep these two straight? Try this mnemonic: the s in sympathetic is for “stress,” because this is your fight-or-flight stress response. The p in parasympathetic is for “peace,” because this is your peaceful, resting state. Thanks to Mark O’Brien for this one.)
Together, these two systems keep your body tuned like a guitar string. It’s a mistake to think that when one is active, the other is switched off; actually, they’re both active at all times, merely to different degrees. Although their combined results are directly antagonistic, they’re independent systems, which means that you can have a mixture of a little sympathetic, a lot of parasympathetic, vice versa, a lot of both, or any combination thereof.
Think of it like the hot and cold knobs on your sink. You adjust them separately, but the result is a single water temperature. A little hot and a little cold will give you warm water, but so will a lot of hot and a lot of cold. And if you want to cool it down, you can either turn up the cold, or turn down the hot. Simple.
Well, the secret is that many of the drugs we use in medicine function primarily by adjusting this balance.
A drug that turns up the sympathetic system (thus “speeding you up”) is known as a sympathomimetic. A drug that turns down the sympathetic system is known as a sympatholytic.
A drug that turns up the parasympathetic system (thus “slowing you down”) is known as a parasympathomimetic. A drug that turns down the parasympathetic system is known as a parasympatholytic.
Okay, so those are mouthfuls. But the important thing to remember is that, while they’re not identical, the result of both a sympathomimetic and a parasympatholytic will be to support your fight-or-fight responses (run from the lion!), and the result of both a parasympathomimetic and a sympatholytic will be to support your rest-and-digest behavior (take a nap!). So whichever end you approach it from, there are still only two important end results here — up and down.
Virtually the entire body is controlled by these systems. If you can keep track of how each organ system is affected when you nudge this balance one way or the other, you’ll be able to understand a great deal of how drugs do their work.
For instance, consider epinephrine itself, which we use in auto-injectors to treat severe anaphylaxis. The life-threatening effects of an allergic reaction are primarily shock, due to vascular dilation, and respiratory distress, due to bronchial constriction. Epinephrine is a sympathomimetic (okay, “mimetic” means “mimick,” and epinephrine is actually one of the body’s own sympathetic hormones, so it’s not really mimicking anything — but bear with me here). So it produces a fight or flight response. What is the sympathetic effect on the skin and peripheral vascular system? Vasoconstriction (to pull blood away from the periphery into the core). What is the sympathetic effect on the lungs? Bronchodilation (to allow for greater air exchange during exertion). So the entire cocktail of epi’s beneficial results in anaphylaxis comes from stimulating sympathetic tone.
What if I shoot some heroin? My breathing will become slower and weaker. My level of consciousness will decrease. I will become generally slowwww, because heroin (like all opiates) is fundamentally a depressant. And my pupils, pleasantly parasympathetic, will constrict — the third hallmark sign of opiate use. Who needs light when we’re relaxing?
Subtypes
Now, not all drugs from the same neck of the woods are identical, of course. The effects of the same neurotransmitters can be radically different depending on where they bind. An important distinction should be made between non-selective drugs like epinephrine, which binds with all of the primary adrenergic receptor sites (alpha-1, beta-1, and beta-2), and selective agonists like albuterol, which primarily binds only at certain receptors (beta-2 in that case). In brief:
- Alpha-1 (properly styled, α1) receptors are mainly in the blood vessels, and cause systemic vasoconstriction. Alpha-1 blockers, or antagonists, therefore cause systemic vasodilation.
- Beta-1 (β1) receptors are mainly in the heart, and increase heart rate and contractility. Beta-1 antagonists therefore slow and reduce cardiac output. (Mnemonic: you have 1 heart.)
- Beta-2 (β2) receptors are mainly in the lungs, and cause bronchodilation. Beta-2 antagonists therefore cause bronchoconstriction. (Mnemonic: you have 2 lungs.)
Naturally, none of these categories tell the whole story of a drug. (If they did, we wouldn’t need so many different ones.) Caffeine, atropine, and crystal meth are all very different drugs, even though they all fall roughly into the category of stimulants. But you can keep track of a good deal of their shared effects by understanding their common nature.
Examples
- Drugs ending in -zepam (or sometimes -zolam — eg. diazepam, triazolam) are benzodiazepines, which have broad sedative effects.
- Drugs ending in -alol (or -ilol, -olol — eg. atenolol, labetalol) are beta blockers, which have a sedative effect, usually localized to the heart via beta-1 antagonism.
- Drugs ending in -erol (e.g. albuterol, clenbuterol) are beta-2 agonists, or bronchodilators; they are stimulants that primarily cause bronchodilation via beta-2 receptors.
Most pain killers, sedatives, and anesthetic agents are depressants.
Note: most common suffixes are only applicable to generic drug names. Trade names are usually unique.
More Drug Families: Steroids and Antibiotics; ACE Inhibitors and ARBs; Anticoagulants and Antiplatelets




Recent Comments