Continued from part 1 and part 2
In the end, all three patients receive spinal immobilization. You transport both pediatric patients to Bullitt Medical Center; the P12 assumes care of the mother and transports her to the same destination. No significant injuries are found upon follow-up assessments; however, when the P12 checks Samantha’s blood glucose, they find it to be 32 mg/dL. They administer D50, normalizing her sugar, which improves her level of consciousness; however, she remains confused and becomes somewhat combative. She does endorse substantial alcohol ingestion, is somewhat unclear on drug use, and continues to deny a history of diabetes.
After transferring care, both crews fill out state-mandated documentation to report child abuse, with regard to the mother driving two young children while under the influence and without appropriate car seats or other restraints. You write your documentation with extra caution, aware that it may eventually be used in a court of law.
Discussion
This was a case where no patient was highly acute, but operational issues required some attention and medical confounders obscured the assessment.
General considerations for MVAs
With any significant MVA (or MVC for “motor vehicle collision,” since the DoT takes the position that nothing is truly accidental), there are several factors we should consider:
- Scene safety. Wherever the scene may be, it’s generally at or near a roadway, and it’s a location that’s already proven itself accident-prone. In this case, we were situated in a truck yard somewhat off the main road. If it were a busier area, and we were first to arrive, we would want to park the ambulance to shield the scene from traffic, and request fire apparatus (for more blocking) and police (for traffic control). We should also consider the presence of chemicals or other hazardous material in an industrial area, which was not a problem here.
- Extrication. The time to request additional resources is early. Heavy extrication, where vehicle frames need to be bent or cut, is usually performed by fire department ladder trucks or dedicated rescue apparatus; in this case, the driver’s door was dented and needed to be popped open (technically “confinement” rather than “entrapment”), and it was handled prior to our arrival.
- Cause. Some accidents happen for obvious reasons, such as inattention. Sometimes they’re due to conditions, such as weather or visibility, which is a good clue that such conditions probably persist and might endanger you as well; protect the scene and be cautious during extrication and transport. Sometimes, accidents have a medical cause, which was the case here.
- Damage. We are clinicians, not mechanics, but vehicle damage can provide clues to injury type and severity. Modern vehicles often develop horrific-looking body damage while yielding minor personal injury; automotive safety science has become quite advanced, and a large part of a car’s protection comes from intentionally crumpling to absorb impact. If occupants are restrained, the vehicle can easily eat up a large amount of shock without anyone suffering significant harm. In this case, we saw a front-left impact at seemingly moderate speed, so we anticipate a head-on type injury pattern with some lateral energy. Damage to the driver’s-side lower dashboard area, plus minor knee injury, suggested a “down and under” rather than “up and over” direction of movement, which is typical for a restrained driver; the windshield was also missing any apparent point-of-impact, which supports this. With the seatbelt and airbag, we were not too suspicious of frontal head injury, but we did look for evidence of lateral head impact against the window or side-wall; we found no obvious head trauma or internal vehicle damage. There was likewise no signs of internal impact from the children in the rear, although we remain suspicious of pelvic or abdominal trauma, since they were wearing lap belts without any torso restraints.
- Number of patients. Life was made easier by the truck driver, who was obviously unharmed and decided to elope from the scene prior to our arrival. Samantha was making vague reference to her brother, but it seemed that he was coming to meet her and was not an occupant. It is somewhat bad form to forget about people, so it’s good to try and confirm these things, and the first-in responders (the fire department in this case) can help.
Assessment
Just like in most cases, the majority of essential information was communicated in the first few seconds on scene.
Our eyeball exam from twenty feet was enough for an initial assessment on the kids. The Pediatric Assessment Triangle is a model for identifying pediatric life threats that focuses on obvious, big-payoff findings rather than details (like specific vital signs) which can be tough to measure. The three components are:
- General appearance. This is overall impression and rough neurological status. Are they conscious? If so, sluggish, alert, groggy, engaged with their surroundings, tracking with their eyes? Is there any muscle tone or are they limp? Are they crying? If so, are they consolable? Do they look sick or well?
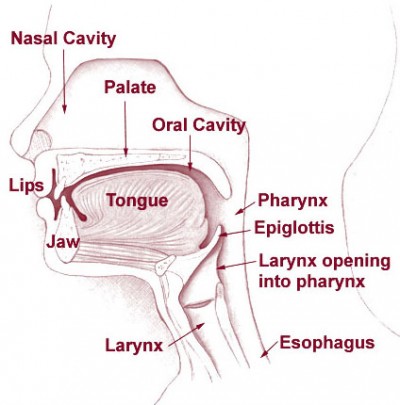
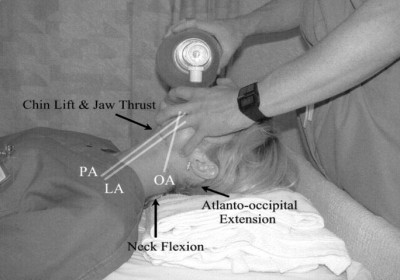
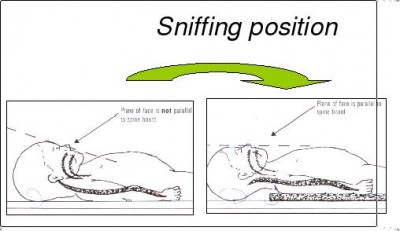
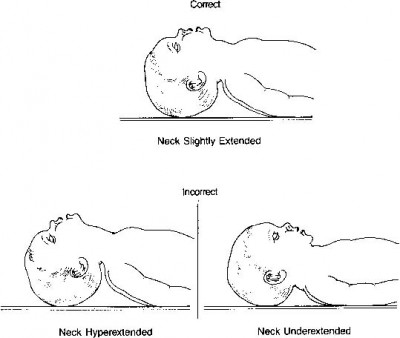
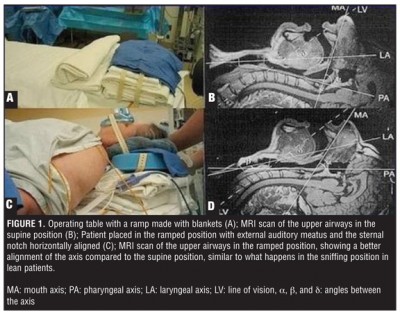
- Work of breathing. This is respiratory assessment. Is the child struggling to breathe? Are they tripoding or assuming a sniffing position to maintain an airway? Is there accessory muscle use, pursed-lip breathing, nasal flaring, chest retractions? Are grossly adventitious breath sounds audible (i.e. wheezing, stridor, grunting, snoring)?
- Circulation. This is general circulatory status. Is skin pink and warm? Is there clear cyanosis, pallor, mottling? Obvious bleeding?
From the first moments on scene, we were able to observe that the pediatric patients were: conscious, crying loudly (therefore with a patent airway and adequate breathing), generally unhappy but not acutely distressed, without obvious bleeding or other trauma, and with normal skin signs. That’s plenty for the initial triage — a more full assessment will come later, but it’s unlikely that we’ll uncover any true life threats.
How about mom? We initially notice no obvious issues except for an altered mental status, which may be masking other problems (such as pain or neurological deficits). We also don’t know the cause of the AMS. Is there alcohol involved? Probably: she directly endorsed this. Drugs? Perhaps: vehemently denying drug use is not uncommon in drug users, and there were purpura consistent with needle “track marks” on her arm. But even if present, neither of those precludes a concomitant traumatic head injury; drunk and high people can bump their head too. And we were reminded of the first rule of EMS: everybody is diabetic. Although the circumstances didn’t necessarily suggest hypoglycemia as the most likely cause, it fit the presentation, and all drunk patients are somewhat at risk for this complication. If she’d stayed in our care, glucometry would have been wise during transport.
Is spinal immobilization needed? Local protocol comes into play. The children are probably low risk. The mechanism as a whole is potentially risky, due to the possibility of side-on energy transfer and head injury, but generally is not too alarming and the assessment findings are fairly reassuring. In the case of the mother, she is the classic example of a poor reporter who cannot reliably describe neck or back pain or participate in a neurological exam; most selective immobilization protocols (such as NEXUS or the Canadian C-spine rule) would advise immobilization in such cases. In this instance, due to equipment shortcomings, one child was immobilized via KED and the other two patients immobilized to long boards, with towel rolls used liberally. The children were liberated almost immediately after arrival at the ED, after a clinical exam by the pediatric emergency physician. The mother began fighting her board after she was roused with D50.
Transport and documentation
This case highlighted the need for intelligent patient assessment to guide transport destinations. Although low-acuity pediatric patients can sometimes be assessed in an adult ED, it depends on the receiving physician’s level of comfort, so in many cases they’ll prefer to transfer them to a specialty center (and any time a patient has to be transferred from where we brought them, we’ve failed them somewhat).
In a similar vein, acute patients needing surgical intervention should always be delivered to trauma centers. Does mom need a trauma center? Since we’re unable to rule out a traumatic cause for her mental status, it’s probably wise, although perhaps not essential. Do the kids need a pediatric trauma center? Probably not; they are, by all appearances, doing fine. Finally, although we could transport parent and kids to different hospitals, it would be distressing to everyone and create logistical headaches (involving consent, billing, and other concerns), so Bullitt Medical Center (an adult trauma center as well as a pediatric ED, although not a pediatric trauma center) is a sensible destination. (Since it’s a larger hospital, it’s also more capable of sustaining the “hit” of receiving three patients simultaneously than a small community ED.) Since the mother is a more challenging patient, it makes sense for the paramedics to take her while our BLS unit acts as a bus for the kids.
As for documentation, depending on state law we may be required to report all instances of child abuse to protective agencies. (In this particular region, reporting is mandated for any child or elder abuse.) If so, local procedures should be followed; although the hospital will most likely perform such reporting as well, in many states this does not absolve EMS of its own responsibilities.
When documenting the call, be aware that charges may be pursued against the mother for neglect, driving under the influence, or other offenses. These may hinge upon your documented findings, such as altered mental status, lack of appropriate child restraints, or statements about substance use. Depending on local laws for mandated reporters, you may be required to report these findings directly to police, or you may actually be prohibited from doing so by HIPAA laws; in either case, however, they should be noted in your report.





Recent Comments