Man’s leaning against a wall. He doesn’t move for hours. Just stands there not moving. Finally, someone says, “You been here all day — don’t you have anything to do?”
“I’m doing it,” he answers.
“Doing what?”
“Holding up the wall.”
And who’s to say he’s not? Maybe he’s working as hard as he can to make sure that wall doesn’t fall down.
In this situation, the man is a compensating mechanism. He is struggling to prevent changes in the wall; keeping that wall upright is an endpoint he cares to maintain, to sustain, to keep intact.
How do we know that the wall isn’t holding up the man? Because we don’t care about the man. Whether he leans or falls doesn’t matter much to anybody. But it would be a terrible thing if the wall collapsed. So we’ll let the man lean or shift in order to prop up the wall when it starts to totter — we’ll use him, adjust him, to compensate for any wall-changes. That’s why he’s there.
If the wall gets weak enough or tilts too far, though, he won’t be able to keep it up. He’ll try, but he’s not infinitely strong, and then maybe the wall begins to tilt or collapses completely. Since we know that under normal circumstances, he’s doing his best to prevent this, if we walk in and see that the wall is tilting, that is not a good sign. It may mean that despite his best efforts, the man has exhausted his strength and is no longer able to resist further wall-changes; or it may mean that, for some reason, the man isn’t doing his job properly. Either way, any further tilting will be unopposed, and will probably happen rapidly and uncontrollably.
Compensators and endpoints
This same dynamic plays out within the human body. As we know, living organisms seek to maintain a certain homeostatic equilibrium. We put our vital metabolic processes in motion and we don’t want them to halt or change, despite any insults or fluctuations imposed upon us by our surrounding environment. So our bodies struggle to keep all of our complex systems at an even keel, using a diverse and powerful array of knobs, dials, and other regulatory tools. Not too hot or too cool, not too acid or too basic, not too fast or too slow. Just right.
The kicker is this, however. Some of our physical parameters are more important than others. In other words, while some parameters have room to adjust, others aren’t negotiable, can’t change much, without derailing our basic ability to function and survive. Things like blood pressure (or at least tissue perfusion, for which blood pressure is a pretty good surrogate measure) are essential to life; your pressure can fluctuate a little, but if it drops too low, you are unquestionably going to suffer organ damage and then die. And yet there are many insults that could potentially lower our blood pressure if we let them: if we bleed a little, or pee a little, or don’t drink enough water, or sweat, or even just stand up instead of sitting down. How do we preserve this vital parameter despite such influences?
By compensating, of course. Our body gladly modulates certain processes in order to preserve other, more important parameters. So in order to maintain blood pressure, perhaps we accelerate our heartrate. In an ideal world, it might be nice if the heart were thumping along at — let’s say — a mellow 80 beats per minute. It’ll use little less energy and less oxygen than if it were beating faster. But it’s really important to keep our blood pressure up, and speeding up the heart can increase the pressure, so we gladly make that trade and induce tachycardia. (Many of these compensatory systems are linked to the sympathetic nervous system, our body’s standard “all hands on deck” response to stress and crisis.)
So imagine we find a patient who’s bleeding and notice that he’s tachycardic, with a normal blood pressure. This suggests a compensated shock; the body is using tachycardia to maintain that normal pressure we see; although his volume is lower than usual, the critical endpoint of adequate blood pressure is still intact.
But what if instead, we found him tachycardic and hypotensive? Well, that’s not good. We see that the body is trying to compensate, but we also see that the important endpoint — blood pressure — is falling nonetheless. The body would never intentionally allow that; BP is too important. So we recognize this as decompensated shock. The hypovolemia has progressed so far, and volume is now so low, that he can’t make up the difference anymore — the compensatory slack has run out — and any further decreases in volume will probably lead to an immediate and unopposed drop in pressure. There’s nothing more the body can do on its own; it’s out of rope.
The skilled clinician — or “homeostatic technician” as Jeff Guy says — uses this predictable progression to understand what’s happening in almost any crisis. Because primary insults are initially covered up by compensatory mechanisms, they may not be immediately apparent, and the earliest and most detectable signs of physical insult are usually nothing more than the footprints of the answering compensation. Thus, when when we encounter those, we know to suspect the underlying problem even if it’s not obvious yet. It’s like seeing brakelights flash from cars on the road ahead; even if you can’t see an obstacle yet, you know people are slowing down for something.
Obvious signs of decompensation usually show up late. Once the primary, underlying problem is revealed by failure of the corrective mechanisms, it’s often progressed so far that it’s too late to address. If you wait to brake until you can see the wreck itself, you might not be able to stop in time.
Two signposts for decompensation
There are two great ways to recognize which signs and symptoms connote decompensation.
The first is to understand which physical parameters are endpoints — which functions the body tries to preserve at all costs. These processes are only compromised as a last resort, so if you see them deteriorate, things are in the end-game; the body doesn’t intentionally sacrifice these for the benefit of anything else.
The second clue is more subtle. In this case, you observe a compensatory mechanism (not an endpoint), but find that it’s no longer successfully compensating — it’s failing, and starting to unwind and scale back, rather than doing its job. The changes in the compensatory system are inappropriate, resulting in less of what we need, not more. This happens when our systems are so damaged that they can’t even fix problems and pursue homeostasis anymore; our infrastructure, maintenance, and repair systems are breaking down. Consider this: we saw how tachycardia could be compensatory, but could bradycardia ever be beneficial in shock? Probably not. So if we found a shocked patient with bradycardia (and likely hypotension, the failing endpoint), we should be very alarmed indeed. There’s nothing helpful, compensatory, or beneficial about bradycardia in the setting of shock, so we recognize that the body would never go there on purpose. It’ll only happen when the machinery itself is falling apart.
Consider, for instance, Cushing’s Triad, the collection of signs often encountered after severe traumatic brain injury, when intracranial pressure has increased enough to squeeze the brain out from the skull like toothpaste. The triad includes hypertension, bradycardia, and irregular or slow respirations. What’s interesting is that, while all are a result of increased ICP, one of these is compensatory, while the others are merely the result of damage. Hypertension is the body’s compensatory attempt to force blood into the brain despite the elevated pressure in the skull. But bradycardia and bradypnea simply result from pressure upon the regulatory centers of the brain tasked with maintaining breathing and heart-rate. That’s why hypertension may be seen earlier, while the other two signs won’t usually manifest until the brain is actively herniating. One signals compensation, the other two decompensation.
Of course, there can be other reasons why compensatory mechanisms might fail, or at least exhibit lackluster performance. Some medications or other aspects of a medical history (potentially unrelated to the current complaint) might throw a wrench in the system. For instance, beta blockers (such as metoprolol and other -olol drugs) limit heart-rate as part of their basic mechanism, so patients with beta blockade often have trouble mustering compensatory tachycardia during shock states. That doesn’t mean they’re any less shocked; in fact, it means they’re more susceptible to hypotension, and that you must be especially on the lookout, because you won’t see one of the red flags (a rapid heart-rate) you might usually expect. Elderly patients with many comorbidities are generally not able to muster up effective compensation for anything, so they can deteriorate quickly, and without much fanfare. Ironically, healthy pediatric patients are the opposite: since they’re so “springy” and smoothly functioning, they compensate very well, with few changes in observable endpoints, until suddenly running out of slack and crashing hard because they’re already so far from shore.
Here are a few important compensatory signs, breakdowns of compensatory systems, and vital physical endpoints:
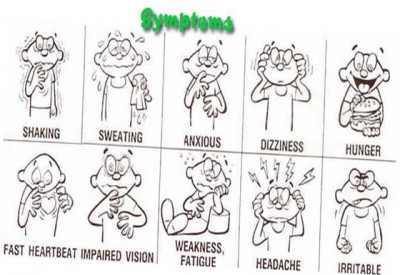
Appropriate signs of compensation
- Tachycardia — increases cardiac output
- Vasoconstriction (cool, pale skin) — raises blood pressure
- Diaphoresis (sweatiness) — decreases temperature when necessary, but is often just a side effect of sympathetic stimulation
- Tachypnea — increases oxygenation, CO2 blowoff, and cardiac preload
- Fever — part of the immune system’s response to infection
- Shivering — warms a hypothermic body
Inappropriate changes in compensatory mechanisms
- Bradycardia — reduces cardiac output, rarely useful in illness; as a chronic finding may be the result of high levels of cardiovascular fitness (in healthy young patients) or medications (in sick old patients); but acutely, it is an ominous finding
- Bradypnea — reduces oxygenation, CO2 blowoff, and cardiac preload
- Hypothermia (or normothermia when a fever is expected) — suggests a failure of temperature regulation
Inviolable endpoints
- Blood pressure — can elevate in stress states, but should not drop below resting levels
- Mental status — except in the presence of a drug or similar agent directly affecting cognition, maintaining appropriate alertness and mentation are always a top priority for the body
- Blood glucose — kept at normal levels in almost all situations, except when the regulatory systems fail, as in diabetes mellitus
- pH — most of the cellular machinery fall apart if significant acidosis or alkalosis occurs
- Low O2 saturation or cyanosis — although oxygen saturation can dip briefly without harm, and in some patients (particularly those with COPD, or long-time smokers) it may run low at baseline, a significant acute drop — or the clinical equivalent, which is frank cyanosis — is always inappropriate.




Recent Comments