Orthostatic vital signs. Nurses think they’re a pain in the neck. Some doctors think they’re of marginal usefulness. Many providers simply think they’re a dying breed.
Like many old-school physical exam techniques, though, they’re dying only because high-tech imaging and laboratory techniques have largely replaced their role. And I don’t know about you, but my ambulance doesn’t come equipped for an ultrasound or serum electrolytes. Diagnostically, EMS lives in the Olden Days — the days of the hands-on physical, the stethoscope, the palpation and percussion, the careful and detailed history. For us, orthostatics have been and still are a valuable tool in patient assessment.
How are they performed? Orthostatic vital signs are essentially multiple sets of vitals taken from the patient in different positions. (They’re also sometimes known as the tilt test or tilt table, which is indeed another way to perform them — if you have a big, pivoting table available. Postural vitals is yet another name.) They usually include blood pressure and pulse, and are taken in two to three positions — supine (flat on the back) and standing are the most common, but a sitting position is sometimes also included, or used instead of standing. This is useful when a patient is unable to safely stand, although it’s not quite as diagnostically sensitive.
Why would we do such a dance? The main badness that orthostatics reveal is hypovolemia. With a full tank of blood, what ordinarily happens when I stand up? Gravity draws some of my blood into the lower portion of my body (mostly these big ol’ legs). This reduces perfusion to the important organs upstairs, especially my brain, so my body instantly compensates by increasing my heartrate a bit and tightening up my vasculature. No problem. However, what if my circulating volume is low — whether due to bleeding, dehydration, or even a “relative” hypovolemia (in distributive shocks such as sepsis or anaphylaxis)? In that case, when my smaller volume of blood is pulled away by gravity, my body will have a harder time compensating. If it’s not fully able to, then my blood pressure will drop systemically.
“But,” you cry, “surely this is all just extra steps. Can’t I recognize hypovolemia from basic vital signs — no matter what position you’re in?”
Well, yes and no. If it’s severe enough, then it will be readily apparent even if I’m standing on my head. But we routinely take baseline vitals on patients who are at least somewhat horizontal, and this is the ideal position to allow the body to compensate for low volume. By “challenging” the system with the use of gravity, we reveal the compensated hypovolemias… rather than only seeing the severely decompensated shock patients, who we can easily diagnose from thirty paces anyway. Like a cardiac stress test, we see more by pushing the body until it starts to fail; that’s how you discover the cracks beneath the surface.
Do we run on patients with hypovolemia? Oh, yes. External bleeding is a gimme, but how about GI bleeds? Decreased oral fluid intake? Increased urination due to diuretics? How about the day after a frat party kegger? Any of this sound familiar? It would be foolish to take the time to do this when it won’t affect patient care — such as in the obviously shocked patient — but there are times when what it reveals can be important, such as in patients who initially appear well and are considering refusing transport.
Here’s the process I’d recommend for taking orthostatics:
- Start with your initial, baseline set of vitals. Whatever position your patient is found in, that’s fine. Deal with your initial assessment in the usual fashion.
- Once you’re starting to go down a diagnostic pathway that prominently includes hypovolemic conditions in the differential, start thinking about orthostatics. If your initial vitals were taken while seated, try lying the patient flat and taking another pulse and BP. If possible, wait a minute or so between posture change and obtaining vitals; this will allow their system to “settle out” and avoid capturing aberrant numbers while they reestablish equilibrium.
- Ask yourself: can the patient safely stand? Even in altered or poorly-ambulatory individuals, the answer might be “yes” with your assistance, up to and including a burly firefighter supporting them from behind with a bearhug. (Caution here is advised even in basically well patients, because significant orthostatic hypotension may result in a sudden loss of consciousness upon standing. You don’t want your “positive” finding to come from a downed patient with a fresh hip fracture.) If safe to do so, stand the patient and take another pulse and BP. Again, waiting at least a minute is ideal, but if that’s not possible, don’t fret too much.
- For totally non-ambulatory patients, substitute sitting upright for standing. Ideally, this should be in a chair (or off the side of the stretcher) where their legs can hang, rather than a Fowler’s position with legs straight ahead.
- For utterly immobile patients who can’t even sit upright, or if attempting orthostatics in the truck while already transporting, you’ll need to do your best to position them with the stretcher back itself. Fully supine will be your low position, full upright Fowler’s will be your high position, and a semi-Fowler’s middle ground can be included if desired.
On interpretation: healthy, euvolemic patients can exhibit small orthostatic changes, so hypovolemia is only appreciable from a significant drop in BP or increase in heart rate. From supine to standing, a drop in the systolic blood pressure of over 20 is usually considered abnormal, as is an increase in pulse of over 30. (Changes from supine to sitting, or sitting to standing, will obviously be smaller, and therefore harder to distinguish from ordinary physiological fluctuations.) A drop in diastolic pressure of over 10 is also considered aberrant. You can remember this as the “10–20–30” rule.
Try to remember what’s going on here. As the patient shifts upright, their available volume is decreasing, for which their body attempts to compensate — in part by increasing their heart rate. It’s a truism that younger, healthier, less medicated patients are more able to compensate than older and less well individuals. So for the same volume status, you would be more likely to see an increase in pulse from the younger patient, perhaps with no change in pressure; whereas the older patient might have less pulse differential but a greater drop in pressure. (On the whole, the pulse change tends to be a more sensitive indicator than pressure, since almost everyone is able to compensate somewhat for orthostatic effects. As always, if you look for the compensation rather than the decompensation — the patch, rather than the hole it’s covering — you’ll see more red flags and find them sooner.)
Are substantial orthostatic changes definitive proof of hypovolemia? No, nothing’s certain in this world. Another possible cause is autonomic dysregulation, which essentially means that the normal compensating mechanisms (namely baroreceptors that detect the drop in pressure and stimulate vasoconstriction, chronotropy, and inotropy) fail to function properly. You do have enough juice, but your body isn’t doing its job of keeping it evenly circulating. Vasovagal syncope is one common example of this; I’ve got it myself, in fact, and hence have a habit of passing out while squatting. This sort of thing is not related to volume status, although if you combine the two the effect can be synergistic. A good history can help distinguish them: ask the patient if they have a prior history of dizziness upon standing.
Finally, pulse and pressure are not the only changes you can assess. One of the best indicators of orthostatic hypotension is simply a subjective feeling of light-headedness reported by the patient. Although sudden light-headedness upon standing can have other causes (the other big possibility is benign paroxysmal positional vertigo — although strictly speaking, BPPV tends to cause “dizziness,” which is not the same as “lightheadedness”), hypovolemia is certainly one of the most likely. So stand ’em up when it’s safe and reasonable, ask how they feel, grab the vitals if you can, and maybe even take the opportunity to see how well they walk (a nice, broad neurological test — the total inability to ambulate in a normally ambulatory patient is a very ominous sign).
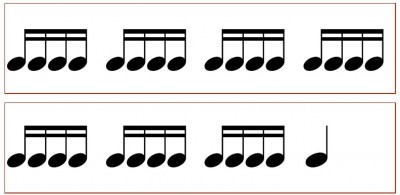
Orthostatics are usually recorded on documentation by drawing little stick figures of the appropriate postures. For those who find this goofy, or are documenting on computers without “stick figure” keys, a full written description will do.



Recent Comments