Understanding the renin-angiotensin-aldosterone system is like following one of those dotted-line Family Circus cartoons — not just long and tortuous, but seemingly designed just to be obnoxious.
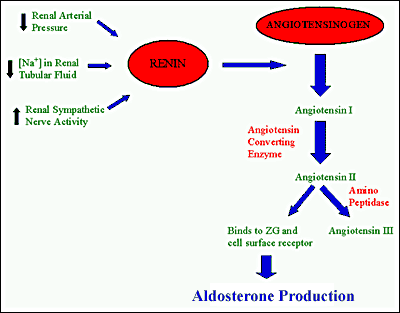
Here’s the basic idea. The RAAS is the basic system your body uses to control blood pressure, as well as related values like fluid volume and sodium levels. The most important thing to understand is that the activation of this system causes an increase in blood pressure. Following the trail:
First, renin is released by the kidneys. Renin attacks circulating angiotensinogen, turning it into angiotensin I. Angiotensin I is attacked by circulating angiotensin converting enzyme (or ACE), which turns it into angiotensin II. Angiotensin II has various effects, one of which is to stimulate the release of aldosterone.
Whew.
But this isn’t as complicated as it looks. Renin has no real effect. Angiotensinogen just makes angiotensin I. Angiotensin I’s main role is to make angiotensin II. The real money here is in angiotensin II, as well as aldosterone.
Angiotensin II has the primary effect of vasoconstriction. It tightens up the vasculature, increasing blood pressure and systemic resistance. It also produces vasopressin (aka ADH, or anti-diuretic hormone) and aldosterone, which cause the kidneys to downregulate urine production — more fluid will be returned to the circulation rather than discarded into the bladder. Vasopressin also helps angiotensin II to induce further vasoconstriction.
To make a long story short, the activation of the RAAS system causes an increase in blood pressure via both vasoconstriction and a decrease in kidney output. It is always active, playing a key role in maintaining homeostasis; if you sweat out a liter of water running a marathon, or bleed out a liter from a gunshot wound, the system simply upregulates itself to maintain your blood pressure using the remaining volume. (Unlike the sympathetic and parasympathetic systems, which also play a major role in regulating blood pressure, regulation via the RAAS is captained mainly at the kidneys, where low pressure and throughput induces increased renin production.)
Cool? Cool.
Okay, so the role of ACE, or angiotensin-converting enzyme, was to transform the useless angiotensin I into the powerful angiotensin II. What do you think a drug called an ACE inhibitor would do? Indeed: it inhibits the activity of ACE, thus reducing the production of angiotensin II, which then causes reduced production of aldosterone and vasopressin.
Less angiotensin II means less vasoconstriction; the systemic circulation opens up, reducing blood pressure. Less aldosterone means less fluid is retained at the kidneys, so urine output is increased, reducing circulating volume, and again, reducing blood pressure. Handy!
A secondary role of ACE is to degrade, or break down, bradykinin. Bradykinin is basically just another vasodilator. If ACE is inhibited, then less bradykinin will be broken down, hence more bradykinin will be available. The result is more vasodilation — once again, reducing blood pressure.
Readers who can recognize patterns will probably have deduced that ACE inhibitors are used primarily to reduce blood pressure. Obviously, this includes the typical patient with primary hypertension that needs to be managed to reduce long-term morbidity. But it also means other things:
- Reduced afterload — the resistance the heart has to push against when it pumps blood — means less work for the heart. This is beneficial for patients with heart failure, whose hearts aren’t pumping very well to begin with; or with coronary artery disease, whose hearts need to manage their workload to match the oxygen they’re able to bring in. It reduces “remodelling,” where the heart and the arteries thicken and change shape to better pump hypertensive volumes, with harmful results. And it reduces the damage following myocardial infarction.
- Reduced preload — the amount of blood that passively fills the heart during diastole — — also means less work for the heart. Greater preload causes greater filling and hence greater contraction, which all means more work, more oxygen demand, and more remodelling. In heart failure, where the heart is unable to fully expel its contents, reduced preload also means less “extra” fluid to back up into the lungs and circulation, and therefore less edema.
- Better renal function. This is a desirable effect in patients with various forms of kidney disease.
Angiotensin receptor blockers (ARBs) are a closely related family of drugs. Instead of interfering with the conversion of angiotensin I to angiotensin II, they simply prevent angiotensin II from binding with its receptors. The effects are therefore largely the same: vasodilation; reduced aldosterone production, with corresponding greater urine output; and reduction in hypertension with less work for the heart.
The main difference between ACE inhibitors and ARBs goes back to bradykinin. If you remember, ACE plays two roles: converting angiotensin I to angiotensin II, and degrading bradykinin, a vasodilator. Since ARBs have no effect on ACE, bradykinin is broken down normally. This may result in slightly less vasodilation, but it also reduces the side effects of elevated bradykinin, which can include edema and a nasty cough. ARBs are most often used in patients who can’t tolerate ACE inhibitors.
Overdose on ACE inhibitors is generally unremarkable. The main effect is hypotension, but it is rarely severe.
Examples
Generic names of ACE inhibitors and ARBs are very, very easy. Trade names are harder, but do have some common elements.
ACE inhibitors
- Drugs ending in -pril are invariably ACE inhibitors (enalapril, ramipril, captopril, lisinopril, etc.)
- Drugs ending in -ace are often trade names of ACE inhibitors (Altace, Tritace)
- Drugs ending in -tec are often trade names of ACE inhibitors (Vasotec, Renitec, Novatec)
ARBs
- Drugs ending in -sartan are invariably ARBs (losartan, valsartan, candesartan, etc.)
More Drug Families: Stimulants and Depressants; Steroids and Antibiotics; Anticoagulants and Antiplatelets
Wow. Very easy to understand. Thanks a bunch! I’m a nurse blogger and I would like to use this as a reference to my posts and lectures, if it’s okay. I would also like to commend on your writing style… 🙂
Thank you so much, so helpful with revision!!