Continued from Mastering BLS Ventilation: Introduction, then Mastering BLS Ventilation: Hardware, then Mastering BLS Ventilation: Core Techniques, and finally Mastering BLS Ventilation: Supplemental Methods
Over the past few weeks, we’ve explored a large number of BLS tools for maintaining a patent airway and pushing oxygen through it. This is good, because the only reliable way to address this dilemma is by having a large toolbox. Nobody can oxygenate every patient with just one trick, no matter how skilled they are.
But a box of tools isn’t an approach to the airway, no matter how big it is. It’s just a box. You need more than that — you need a plan. If I toss you an apneic person, what are you going to do? What if that fails? What’s plan B? And plan C? Then what happens?
The only way to answer these questions is by creating your own scheme, a roadmap to fall back upon. I can’t give it to you, because I don’t know your variables. I don’t know your specific skillsets, what you’re comfortable with, what you’ve practiced and in what situations, versus what you’ve never done in your life. I don’t know what your local protocols are, and what equipment you have available (including extra toys like supraglottic airways or Narcan/naloxone), your typical transport times, or the general availability of ALS. I don’t know what type of patients you usually encounter, how many personnel you have on hand to manage them, and what sort of extrications are involved.
But you know those things. Roll it all into a ball so you understand your resources and challenges, consider the various tools we’ve discussed, and make a plan.
Click here for a PDF version (recommended if printing)
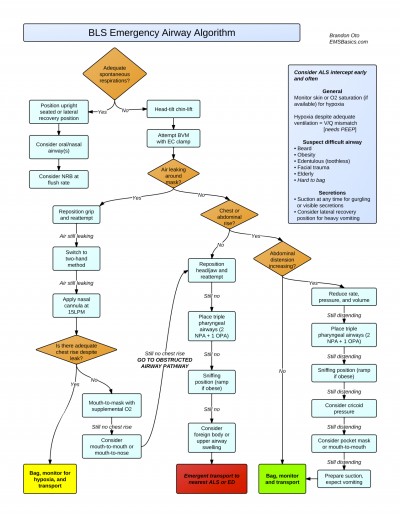
Here’s an example I concocted. This is a flowchart patterned after the airway algorithms commonly used in the ED or the ICU, and it incorporates most of the ideas we’ve talked about. It assumes certain things, so I’m not putting it forward as something to follow religiously. Rather, it’s meant as an example: this is the type of thinking you need to be doing. You probably won’t take the time to chart it out, but you should at least be thinking about it now, because figuring it out on scene with the sick person is too late. Mentally walk through what you’d do at each juncture, imagining yourself treating a real patient in your real ambulance using your real gear. Think about your responses to each dilemma, and if you discover you’re unsure about any details, seek out additional training or practice to patch those holes; for instance, spending some time with a (high quality) mannequin and a BVM can be beneficial. Even just a few minutes playing with the BVM (try bagging yourself until you really understand how the pressures and airflows work), the non-rebreather, your various airways, and so forth can help develop familiarity with little-used tools, so you truly understand how all the valves function, how to size and adjust everything, even where it can be found in your bags. This is particularly important if you rarely use these tools, because infrequent or not, you still need to exhibit mastery when the time comes.
Questions, comments, or remarks on our proposed model are welcome.
Thanks for sticking with us through this exploration of the art and science of BLS ventilation.
Da girare…