This past weekend, I was able to attend the Western Massachusetts EMS Conference alongside such luminaries as Scott Kier and Kyle David Bates (of the extraordinary Pedi-U podcast). We sat through two days of outstanding lectures on various EMS-related topics, and walked away with some ideas and information I haven’t found anywhere else. Here are just a few of the unique pearls from the conference. Thanks to everyone for the great time!
Kyle David Bates on Mechanism of Injury
- In an MVC, ejected (that is, fully ejected) victims have a 1/3 chance of a cervical spine fracture.
- They also have around 25 times higher chance of mortality than an equivalent non-ejected patient.
- Is “another death in the same vehicle” a legitimate concern when considering mechanism? Yes, but make sure that death wasn’t from an localized cause—for instance, a girder in the face, or they had a heart attack before they crashed.
- How about “intrusion”? Over twelve inches into the patient compartment where your patient is found (meaning, visible from inside—not from the outside, which includes the buffer space of the walls), not including areas like the hood, trunk, etc. Alternately, over 18 inches into the patient compartment in areas where your patient is not found—for instance, the rear seating area, when you’re treating the solo driver.
- “Distracting injuries” can mean painful injuries that distract the patient, but also gross stuff that distracts the provider. Consider a head-to-toe on virtually everyone, even when the funky arm fracture is drawing your attention.
- Many “trauma” patients are no longer being treated with surgery anyway, so sending everything to the trauma centers overloads them for no reason.
- One more reason why the sternal rub is not a great diagnostic: if they do clutch at their chest in response, is that localizing—or an abnormal, decorticate flexion response? Different GCS scores, but you can’t tell.
- Are extremity injuries significant mechanisms? Penetrating injury proximal to the elbows or knees should be considered threatening to the torso, so yes. Pelvic fractures? For sure. (“How much blood can you lose into your pelvis? All of it!”)
- With the automobile safety technology available today, you can crash fast, turn your car into a paperweight, but walk away unharmed. We no longer care about “high-speed,” only “high-risk,” which has many factors (see the Rogue Medic’s recent post on this).
- Auto vs. pedestrians: kids get upper body injuries; adults get lateral trauma as we turn and try to get out of the way. Both can get run over.
- Motorcycles. Harley-type riders seem to have more head injuries: they get hit by cars, due to low profile and dark clothing, and they wear partial helmets. Sports bikes get more extremity injuries: they wear good protection, are higher visibility, but they ride fast and run into things, breaking any and every bone they have.
- Rollovers: no longer trauma criteria. You can roll and do great if you’re restrained. Number of rolls, final position, even roof intrusion have no correlation to injury severity.
- Extrication time >20 minutes: no longer trauma criteria. Sometimes it just takes a while due to weather, access, etc, and newer vehicles are supposed to crumple more anyway.
- Are burns trauma criteria? No. If they need specialized care, it’s a burn center, but this is not that time-sensitive—more a long-term management thing—so someone with burns and trauma should go to the trauma center instead, can be transferred later for burn care.
- Helicopter transport: costs can range from $2,000 to $20,000 depending on distance, and insurers are refusing to pay many of these bills due to lack of necessity. Also consider the possibility of everyone dying in a fiery crash. Weigh cost vs. benefit.
Kyle David Bates on Shortness of Breath
- Anxiety is caused by hypoxia; the cure for this is supplemental oxygen.
- Sleepiness is caused by hypercapnia; the cure for this is bagging.
- OPA or NPA? Testing the gag reflex may create a bigger airway problem (vomit). Better yet, check the mouth for pooled saliva; if present, there is no gag, use an OPA. If absent, they have a gag and are managing their own secretions, use an NPA.
- Respiratory distress means there’s a problem, but they’re compensating (compensatory signs like tachypnea).
- Respiratory failure means they’re decompensating (hypoxic/hypercarbic signs like altered mental status, cyanosis, falling sats)
- Respiratory arrest means they’re not breathing.
- Normal inspiration:expiration cycle about 1:2. Obstructive pulmonary problems impede expiration first, because that’s the passive process—it’s easier to inhale past obstructions because it’s an active process. So asthmatics have ratios like 1:4 or 1:5, they’re using active exhalation, and using auto-PEEP maneuvers. (Pursed lips in adults, grunting in kids.)
- In adults, look for retractions intercostal (between the ribs) and sternal notch (between the clavicles); in kids, look substernal (below the ribs).
- 40% of patients hospitalized with asthma have a pneumothorax! (Not necessarily clinically significant, though.)
- Pulsus paradoxus/paradoxical pulses are a useful early sign of significant pulmonary dysfunction.
- 90% of asthma attacks linked with an allergic reaction; however, rhinovirus (the common cold) may now be a contender. Others include: exercise (not sure why; maybe the temperature differential), active menstruation (asthma very common in young post-pubescent women—maybe the hormones), psychological (stress, panic), aspirin use.
- Kids compensate great, so cyanosis (a decompensation sign) in kids is very late and very bad.
- Risk-stratify these patients, because high risk patients can decompensate fast even if they look okay now. Previous hospitalizations? ICU admits? Intubations?
- Cough asthma: no dyspnea, just dry coughing. It happens.
- Smokers: measured in pack-years. 1 pack a day for 20 years is 20 pack-years, 2 packs a day for 5 years is 10 pack-years; 30–35 pack-years is where we start to see bad dysfunction.
- Best place to check skin? Under the lower eyelid—lift it and check the mucus membranes. Dry for dehydration, pale for shock, blue for cyanosis, the whole gamut.
- Ascites is a sign of fluid overload; try the fluid wave test. (Scroll down to “Examining for a fluid wave” here.)
- Nebulized ipratropium/Atrovent: its role is mainly to reduce mucus and secretions (cf. atropine). Tachycardia etc. is not a contraindication, because it’s not absorbed systemically; it remains in the lungs.
- Give nebs by hand-held mask or T-piece instead of strapping it to their face; that way you have a warning of deterioration when they can no longer hold it to their face.
- Bronchodilators may not work great in beta-blocked patients.
- Steroids take hours to have an effect, but the earlier they’re given the better the outcomes; give ’em if you have ’em.
- If they need RSI, ketamine is nice because it also bronchodilates.
- “Facilitated intubation” (i.e. snow ’em with a ton of benzos/narcs)? Be careful, because if you don’t get that tube, it’ll take forever to wear off; these aren’t short-duration drugs.
Kyle David Bates on Pediatrics
- Use the Pediatric Assessment Triangle! Appearance, Work of Breathing, Circulation.
- Appearance: General activity level and impression. Muscle tone, interactivity and engagement, look/gaze, crying. Appropriate appearance depends on age. Indicates a CNS/metabolic problem. (Make sure to check their sugar.)
- Work of Breathing: Flaring, retractions, audible sounds, positioning. Remember they’re belly breathers.
- Circulation: mostly skin. Cyanosis (bad), pallor, mottling (pallor + patchy cyanosis), marbling (in newborns—bright red skin with visible blood vessels, maybe some white areas—this is normal). Check cap refill on bottom of foot in little kids.
- Shock in kids is most often from dehydration.
- Airway: crying is a great sign. Remember to pad under the shoulders when lying flat, their huge heads can tip them forward and block the airway. Avoid NPAs in infants. In very small kids, breath sounds can transmit, so you may hear upper sounds in the chest or chest sounds in the trachea.
- Under 2 months: peripheral cyanosis is normal, central cyanosis is bad. Limited behavior, often won’t visually track. Ask parents if their behavior is normal. Ask about obstetric history, it’s still relevant. They have no immune system really, so any infection (temp over 100.4) is a serious emergency.
- 2–6 months: social smile, will track visually, recognize mom, strong cry and can roll/sit with support. May still be okay with strangers, but try to keep them with parents; if parents like you, they’ll like you
- 6–12 months: stranger anxiety (unless they’re raised very communally). Very mobile and explore with their mouth, so always think about foreign body airway obstructions, especially up the nose, especially for dyspnea with sudden onset. Separation anxiety, so keep with parent. Offer distractions (toys, etc.). Do exam from toe to head so they get used to you before you reach their face.
- 1–3 yrs (toddlers, “terrible 2s”): mobile, curious, opinionated, ego-centric, can’t abstractly connect cause-and-effect but learn from experience. Keep with the parents, distract them, assess painful part last (or everything you touch afterwards will hurt). May talk a lot or not much, it’s all normal, but they always understand more than they let on, so be careful what you say.
- 3–5 yrs (preschool): magical thinkers, misconceptions (“silly” ideas like if they leak too much they’ll run out of blood), many fears (death/darkness/mutilation/aloneness), short attention span. Explain things in simple terms, relate to them (any cartoons or toys in the house you recognize?), use toys, involve them (here hold this, which arm should I use, etc). Don’t ever negotiate, just tell them what to do; praise them often; never ridicule.
- 6–12 yrs (school aged): talkative, mobile, may not get cause and effect, want reassurance, involvement, praise. Live in present, may not think about danger or risk. Peer involvement. Speak directly to them, anticipate questions (will this hurt? am I going to die?), give simple explanations, don’t ever lie, respect privacy. If you need to do something painful (IVs, etc.) don’t tell them until just before, or they’ll dwell on it. Head-to-toe okay.
- 13–18 (adolescents): regress when hurt or sick—act like big toddlers. Can understand and theoretically have common sense, but still take risks. Peer support. Speak directly, give concrete explanations, respect privacy, have patience.
- Under 21 usually considered “pediatric.”
- Degree of fever temp not associated with severity. No actual danger to brain until 106–107 degrees F or so.
Dr. Lisa Patterson on Trauma and Field Triage
- RR <20 in infants is trauma center criteria since this is the one easily-measurable vital sign for them.
- Crushed/degloved/mangled extremities: although not life-threatening, still worth the divert, because usually needs multi-specialty care (plastic surgery, orthopedics, hand specialists, etc.) to maximize function.
- Calling in “altered mental status” or “unresponsive” is not super helpful—give a GCS or otherwise specify what you mean, there’s a big range here.
- Trauma activations here are typically three tiers: category 1 (life threat), category 2 (no immediate emergency, but some concern or suspicion due to mechanism or presentation), consult (no concern on initial presentation, but later decision to admit, trauma paged down to consult).
- Activation may alert/standby numerous parties including radiology, OR, pharm, blood bank, lab, ICU, respiratory, anesthesiology, social workers, etc. Not a small thing.
Sean Dorr on OEMS investigations
- [This is Massachusetts-specific information; local providers can contact me directly if they want to hear about some of this material.— ed.]
Ginnie Teed on Organ and Tissue Donation
- Donation is hugely hugely valuable and lifesaving, but there’s not nearly enough. About 60-70% of Americans are registered donors, around 100 million people, but only 1% end up as usable donors and we need far more. Low rates aren’t from consent, they’re from the logistics of getting viable candidates.
- Uniform Anatomical Gift Act (UAGA) is federal regulation providing basic requirements for process; states use this standard to form their own systems. Registered donors must be recognized and organ procurement agencies are required to advocate for them even against wishes of family, etc. Driver’s license “opt-in” now considered legal consent in some but not all states.
- National Organ Transplant Act establishes the rules of the registry, blinds the entire process, prevents manipulation or line-jumping; the database is centralized and controlled; you can’t legally buy or otherwise get around the system. Manipulation is taken very very seriously and massively investigated, because it’s not only unethical, the pall it casts over the process makes others decide not to donate—the result is many lives lost.
- Referrals (i.e. calling procurement organization to say, “we have a potential donor”) come from hospitals, nursing homes, clinics, whomever. This process is exempt from HIPAA.
- Tissues tested more heavily than organs, because if an infection is carried through transplanted (i.e. nonliving) tissue, it’s almost impossible to eradicate.
- Organs used: vital organs. Heart, lungs, kidneys and livers (most common), pancreas, sometimes small bowel. Max 9 organs per donor.
- Tissues used: not living, usually good for about 24 hours after death. Bones (not marrow, which is living), although we try to not obviously mutilate people (for their family’s sake), skin (hugely beneficial), corneas, vessels, heart valves, pericardium, connective tissue (for orthopedic repairs).
- Three ways to declare death: neurological (no brain activity; body only alive due to our mechanical support; recovery team responds to site and performs planned recovery); cardiac death (heart stops; not planned); planned extubation/cardiac death (patient is mechanically supported, determination made that there is no possibility to survive on their own; vent is pulled, if heart stops within 59 minutes they can take some organs; usually just the durable liver and kidneys unless bypass is available).
- Live organs can only be taken from perfused patients. Someone “dead” (i.e. no pulses) can be a tissue donor but not an organ donor unless you get ROSC. No point in continuing CPR to “maintain the organs” if there’s no possibility of getting return of circulation.
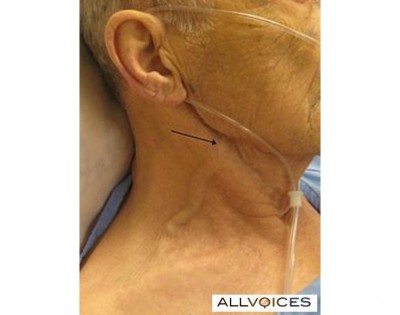
- EMS documentation absolutely critical for determining donor eligibility. Need to know downtime in arrests, how much CPR, any ROSC no matter how brief, events/mechanism leading to arrest. There are hard limits on fluid/blood/colloids received, so they must know how much fluid you gave (reasonable estimate is fine). Must document all needlesticks, number and location; if they find any holes that aren’t accounted for they’ll have to assume they’re a drug user or that additional lines were started and extra liters given. If you don’t want to document something at least tell the receiving staff.
- If blood is drawn, label must be placed so that expiration date of tube is still readable (FDA requirement).
- Every donor can save up to 200 people; failure to document can kill just as many.
UMass Memorial LifeFlight on Air Ambulance Transport
- Consider: how do you want the helicopter used? Need their higher level of care? Rapid transport to trauma center? Transport multiple patients in an MCI to more distant hospitals to reduce burden on closest facilities? Can even split the crew to provide higher level of care for multiple ground ambulances.
- Many services simply will not fly into a hazmat situation.
- Best makeshift landing zones are schools—big open areas, everyone knows where it is.
- Wires are a major hazard, make sure to warn pilot—you can see them but he can’t.
- Need about 100 x 100 ft for an LZ, or 35–40 big-ish strides per side. Secure the area against bystanders.
- Hazards to clear, alert the pilot to, or just pick another spot: poles, antennas, trees, bushes, livestock, stumps, holes, rocks, logs, mile markers, debris. Tall grass can hide hazards. Close all vehicle doors, put your chinstraps on, secure loose items. Don’t stare at the bird landing, turn your back and watch for hazards.
- Bad surfaces are dust, dirt, snow, ice, hay. Snow should ideally be very fluffy or very packed. If they land and get iced they may not be able to take off again. Don’t wash down a dusty LZ unless pilot requests it. Paved areas are simplest and best. Large clear roadways can land multiple choppers in a row.
- Lighting options: orange traffic cone at each corner, with a handlight placed in each at nighttime. Or, flashing ministrobe at each corner. Or, vehicle headlights crossing the LZ. Don’t shine anything up at the helo, don’t mark with loose material, don’t use flares.
- Designate one person as LZ Command (not the IC). Nobody else communicates with the helicopter. Your portable radio probably won’t reach them; use the mobile in the truck. If there’s any hazard on final approach, say one word—”STOP”—and pilot will abort.
- Most crashes are pilot error, and most pilot error is due to fatigue. There should be hour limits for a pilot, and this is a valid reason to refuse to fly.
Detective John LeClair, EMT-P, on Opiates and Prescription Pills
- Heroin is still big, but pills are a huge player now too. You get an easy prescription from a walk-in clinic or ED, pay maybe a couple bucks with Medicare/Medicaid, and can not only sell them for easy cash but can crush and snort/shoot it for the same effect as heroin. Then if money or access runs low, you end up on heroin anyway to chase that high.
- Oxycontin/oxycodone best selling narcotic in the nation ten years ago, but now on the wane. You scrape off the time-release coating, crush it and snort or chew it. “Hillybilly heroin,” “blue,” “oxycotton,” “kicker,” etc. Street price about $1/mg (40mg, 80mg, 160mg common), so many turned to crime. In Aug 2010, manufacturer (Purdue) added a “geling” agent which turns it to gel when it contacts water, making it difficult to snort. Try to snort this Oxycontin OP and it turns into a ball in your nose. Some people are sticking straws/tubes up in there to try and get it deeper and deeper, so airway obstructions are happening.
- Percocet: oxy plus acetaminophen. For years the most common analgesic for sports injuries, so common among youth. Kids shared ’em, put out bowls of them at parties, girls prostituted themselves for pills. Taken with alcohol the APAP/Tylenol kills your liver. “Littles,” “little babies,” “little dogs.”
- Opana/oxymorphone: getting popular after Oxy OP started ruining everyone’s fun. Same idea but you can still snort it. Twice as strong, and costs twice as much ($2/mg)
- How to grind? Take a hose clamp, cut it, straighten it, tape it down, run the pill across the holes to grind it. Or use a Pedi-Egg, which collects the powder for you. The finer, the better high.
- Heroin: snort, “skin pop” (subcutaneous), mainline. Must be pretty pure to snort, which it now tends to be, so popularity grew (people were afraid of needles due to HIV). However now some HIV/Hep is spreading through bloody noses and sharing straws anyway.
- Smack, horse, china white, chiva, junk, H, tar, black, fix, dope, brown, dog, food, negra, nod, white horse, stuff. Dealers have their own “brand names.”
- Heroin addicts are creatures of habit; get high same place, same way. Any change in their routine (e.g. different location) can get them amped up, changing their sensitivity and leading to OD even with their usual dose. Consider this if you find an OD somewhere like a car or alley.
- “Cotton fever”: they pluck out wads of cotton from cigarette filters and drop it in the heroin to help filter it. Sometimes when they draw out the liquid they get a bit of cotton, and when they shoot it they get a sort of phlebitis/infection/sepsis.


Recent Comments